Cannabis
| Summary sheet: Cannabis |
| Cannabis | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chemical Nomenclature | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common names | Cannabis, THC, Marijuana, Weed, Pot, Mary Jane, Grass, Herb, Green, Bud, Tree. More names, and slang. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Routes of Administration | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Interactions | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2C-T-x | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2C-x | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5-MeO-xxT | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Amphetamines | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| aMT | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cocaine | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| DMT | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| DOx | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| LSD | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mescaline | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mushrooms | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25x-NBOMe | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Lithium | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Cannabis (also known as THC,[1] marijuana,[2] weed,[3] pot,[4] grass,[5] hemp,[6] zaza,[7] kush,[8] and many others) is a preparation of the cannabis plant that produces psychoactive effects when consumed (via smoking, vaporizing, or ingestion). It is the most used illicit substance in the world.[9][10] The mechanism of action is binding activity at cannabinoid receptors distributed throughout the body.[citation needed]
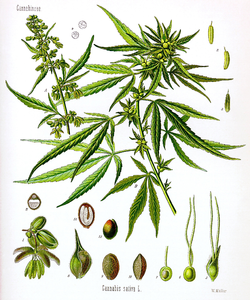
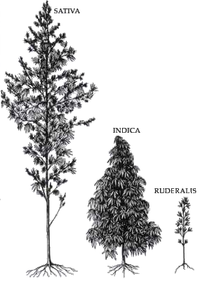
The principal psychoactive constituent of cannabis is tetrahydrocannabinol (THC), which makes up one of 483 known compounds in the plant,[11] including at least 84 other cannabinoids such as cannabidiol (CBD), cannabinol (CBN), tetrahydrocannabivarin (THCV),[12][13] and cannabigerol (CBG). At least three species are recognized: Cannabis sativa, Cannabis indica, and Cannabis ruderalis.[citation needed]
The earliest recorded uses of cannabis date from the 3rd millennium BC.[14] In modern times, cannabis is used for recreational or medicinal and religious or spiritual purposes.[15] It played a central role in the 1960s youth counterculture movement and is associated with the art and music of this era.[citation needed]
Subjective effects include sedation, appetite enhancement, immersion enhancement, creativity enhancement, increased sense of humor, increased music appreciation, visual disconnection, and euphoria. The effects can vary widely depending on dose, strain & form, tolerance, and set and setting. Notably, it can either strongly suppress or enhance anxiety depending on the individual and situation.
Lower doses are associated with relaxing effects similar to a depressant. Higher doses are associated with mild-to-moderate hallucinogenic effects such as visual hallucinations, conceptual thinking and time distortion, as well as a greater risk of anxiety, paranoia, and delusions.
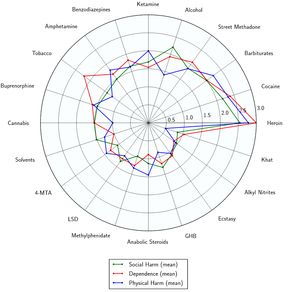
Cannabis is considered to have low to moderate abuse potential.[citation needed] Chronic use is associated with escalating tolerance and psychological dependence in some individuals.[citation needed] It has very low physical toxicity and is essentially impossible to physically overdose on. However, it is capable of exacerbating certain mental health symptoms like delusions or psychosis in predisposed individuals (see this section).[citation needed]
Long-term cannabis use may be associated with negative cognitive effects such as brain fog, lowered motivation, difficulty learning, and inattention. These effects are typically reversible with tapered use and time off.[16]
It is highly advised to use harm reduction practices if using this substance.
History and culture
The genus cannabis is indigenous to central Asia and the Indian subcontinent.[17]
The history of cannabis and its usage by humans dates back to at least the third millennium BC in written history, and possibly as far back as the Pre-Pottery Neolithic B (8800–6500 BCE) based on archaeological evidence. For millennia, the plant has been valued for its use for fiber and rope, as food and medicine, and for its psychoactive properties for religious and recreational use.
The earliest restrictions on cannabis were reported in the Islamic world by the 14th century. In the 19th century, it began to be restricted in colonial countries, often associated with racial and class stresses.
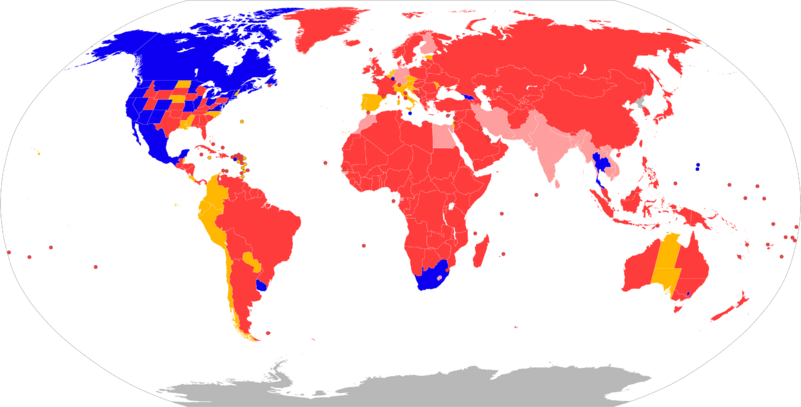
Since the early 20th century, cannabis has been subject to legal restrictions with the possession, use, and sale of cannabis preparations containing psychoactive cannabinoids currently illegal in most countries. However, there is a recent growing trend towards decriminalization and legalization, with the sale of cannabis made legal in some US states and Canada.
In 2004, the U.N. estimated that global consumption patterns of cannabis indicated that approximately 4% of the adult world population (162 million people) used cannabis annually and that approximately 0.6% (22.5 million) of people used cannabis daily.[18] According to the United Nations, it is the most used illicit drug in the world.[9][10]
Potency trends
The potency of illicit cannabis plant material has consistently increased over time since 1995 from ~4% in 1995 to ~12% in 2014. The cannabidiol content has decreased on average from ~.28% in 2001 to <.15% in 2014, resulting in a change in the ratio of Δ9-tetrahydrocannabinol to cannabidiol from 14 times in 1995 to ~80 times in 2014.[19][20]
Etymology
The word cannabis is from Greek κάνναβις (kánnabis) (see Latin cannabis), which was originally Scythian or Thracian.[21] It is related to the Persian kanab, the English canvas and possibly the English hemp (Old English hænep).[21]
Common names
Cannabis has numerous common and street names. The most common ones are: marijuana,[22] weed,[3] pot,[4] grass,[5] hemp,[6], ganja, THC.
Chemistry
Cannabis plants contain a number of different specific compounds at various ratios. Cannabis contains more than 460 compounds;[23] at least 80 of these are cannabinoids,[24][25] chemical compounds that interact with cannabinoid receptors in the brain.[26] The most common cannabinoids are listed below:
Phytocannabinoids
Upon heating, cannabinoid acids decarboxylate to give their psychoactive cannabinoid.
Phytocannabinoid ← phytocannabinoid acid
Quasi-psychedelic phytocannabinoids
- Δ-8-THC. Psychoactive, but about half as potent as Δ-9-THC.
- Decarboxylation: Δ-8-THCA → Δ-8-THC -- only trace amounts exist in cannabis
- Chemical conversion: CBD + acid 8 h → 50% Δ-8-THC
- Δ-9-THC (THC). Most abundant psychoactive component of cannabis. Is the standard when comparing THC analogs.
- Biosynthesis: Tetrahydrocannabinolic acid (THCA) synthase is an enzyme responsible for catalyzing the formation of THCA from cannabigerolic acid (CBGA). GMO yeast with a transgenic placement of a THCA synthase gene from Cannabis will produce THC
- Decarboxylation: THCA (more info) → THC -- The decarboxylation of this compound by heat is essential for the psychoactive effect of smoked cannabis, and depends on conversion of the enol to a keto group when the alpha carbon is protonated.
- Chemical conversion: CBD + acid 8 h → 50% THC
- Δ-10-THC. Psychoactive, but less potent than Δ-8-THC.
- Decarboxylation: Δ-10-THCA → Δ-10-THC-- only trace amounts exist in cannabis
- Chemical conversion: CBD + acid
- Δ-11-THC. Psychoactive, but little is known about this compound.
- THCB (more info)
- THCH (more info). 25 times more potent than THC.
- Decarboxylation: THCHA → THCH -- only trace amounts exist in cannabis
- Chemical conversion: CBDH + acid
- THCP (more info). 30 times more potent than THC.
- Biosynthesis: CBGPA → THCPA → THCP[27]
- Decarboxylation: THCPA → THCP-- only trace amounts exist in cannabis
- Chemical conversion: CBDP + acid
Quasi-psychedelic phytocannabinoids synthesized through chemical modification
- HHC
- HHCH
- HHCP-O-acetate
- THC-O-acetate. 3-5 times more potent than THC.
- Metabolization: THCAO is a prodrug, meaning it requires metabolization in order to take effect. It metabolically undergoes an activation process of converting to THC through de-acetylation, then THC continues into its own primary metabolites similarly to THC's oral route. Because of this, the onset when smoked can be significantly longer ranging from 20-45 minutes, but not as long as ingesting THC orally in comparison. THCAO through the oral route can also have longer onsets than oral THC due to its extra metabolic processes, with an onset of around 90 minutes.[28]
- Decarboxylation: Lack of information on decarboxylation, but it can be inferred that it decarboxylates like its normal parent compound since research suggests that heating it at 340°C (644°F) unbinds the acetyl group, releasing toxic ketene gas.[29]
- Chemical conversion: acetic anhydride + Δ-9-THC/Δ-8-THC → Δ-9-THCAO/Δ-8-THCAO, respectively.[30]
- THCP-O-acetate
Non-quasi-psychedelic phytocannabinoids, some which can be synthesized to quasi-psychedelic cannabinoids with biosynthesis or chemical conversion (see above)
- CBC ← CBCA
- CBCV ← CBCVA
- CBD
- Biosynthesis: CBGA → CBDA → CBD[31]
- Decarboxylation: CBDA → CBD
- Chemical conversion: THC + iodine → CBD
- CBDD
- CBDV ← CBDVA
- CBDH
- CBDP
- Biosynthesis: CBGPA → CBDPA → CBDP[32]
- Decarboxylation: CBDPA → CBDP
- CBE ← CBEA
- CBG
- CBGM ← CBGAM
- CBGV ← CBGVA
- CBL ← CBLA
- CBLV ← CBLVA
- CBN ← CBNA
- CBT ← CBTA
- CBV ← CBVA
- THCC ← THCCA
- Despite sounding a lot like THC, THCC is more similar to CBD than it is to THC
- THCV ← THCVA
- THCV is non-psychoactive.[33]
Pharmacology
The most psychoactive cannabinoid found in the cannabis plant is tetrahydrocannabinol (or delta-9-tetrahydrocannabinol), commonly known as THC.[23] Other cannabinoids include delta-8-tetrahydrocannabinol, cannabidiol (CBD), cannabinol (CBN), cannabicyclol (CBL), cannabichromene (CBC) and cannabigerol (CBG); they have less psychotropic effects than THC, but may play a role in the overall effect of cannabis.[23] The most studied are THC, CBD and CBN.[34]
CYP2C9 genotype affects THC sensitivity significantly:
- Subjects with the *3/*3 genotype had 3-fold higher THC levels in their blood than subjects with the *1/*1 genotype. Those subjects with one copy of each gene (*1/*3) had intermediate THC levels that were about 2-fold higher than subjects with *1/*1.[35]
The entourage effect is a proposed mechanism by which compounds present in cannabis which are largely non-psychoactive by themselves modulate the overall psychoactive effects of the plant (these resulting principally from the action of the main psychoactive component of cannabis, tetrahydrocannabinol (THC)).
THC appears to alter mood and cognition through its agonist actions on the CB1 receptors, which inhibit a secondary messenger system (adenylate cyclase) in a dose dependent manner. Via CB1 activation, THC indirectly increases dopamine release and produces psychotropic effects.
Cannabidiol acts as an allosteric modulator of the mu and delta opioid receptors.[36] THC also potentiates the effects of the glycine receptors.[37] However, the role of these interactions and how they result in the cannabis high remains subject to on-going scientific investigation.
Drugs that activate the CB1 and CB2 receptors are known to upregulate and enhance 5-HT2A receptor activity.[38] The ERK1/ERK2 signaling pathway has been shown to mediate this effect, but the exact biochemical mechanism is unknown. This upregulation and enhancement of the 5-HT2A receptor is why cannabis potentiates the effects of psychedelic drugs and can cause psychedelic effects in very high doses.
Subjective effects
Disclaimer: The effects listed below cite the Subjective Effect Index (SEI), an open research literature based on anecdotal user reports and the personal analyses of PsychonautWiki contributors. As a result, they should be viewed with a healthy degree of skepticism.
It is also worth noting that these effects will not necessarily occur in a predictable or reliable manner, although higher doses are more liable to induce the full spectrum of effects. Likewise, adverse effects become increasingly likely with higher doses and may include addiction, severe injury, or death ☠.
Physical effects 
-
- Sedation[39] - Cannabis may produce a mild sense of stimulation at low to moderate doses. Its effects are primarily sedating and can even be hypnotic. These relaxing properties are suppressed by consciously forcing oneself to engage in physical activities.
In terms of its stimulating effects, these subjective aspects of THC typically last 2-3 hours, whereas the half-life of CBD, which is more relaxing, is 9 hours.[40] Thus, the first dose of cannabis after a period of abstinence will tend to be far more stimulating than subsequent doses, which must compete with the relaxing effects of previous doses.
Because the relaxation both persists much longer and shares many of the same pathways as the stimulation, regular ingestion of THC also leads to increased tolerance to its stimulating effects, but not to its relaxing effects.[citation needed]
- Spontaneous bodily sensations - The "body high" of cannabis is extremely variable and depends entirely on the individual strain as well as dose and method of intake. In general, however, it can be described as a relatively pleasurable, sometimes warm, soft, intoxicating and all-encompassing sensation. At high dosages, it can cause some users to feel shaky or nerve-wracked.
- Appetite enhancement - The feeling of increased appetite following the use of cannabis has been documented for hundreds of years[41] and is known colloquially as "the munchies". Cannabis has been shown in recent studies to stimulate the release of the hormone ghrelin which is normally released by the stomach when empty as a signal for the brain to search for food.[42]
- Appetite suppression - This effect may present itself at the very beginning of the intoxication and is likely due mostly to the cannabinoid THCV.[43]
- Gustatory enhancement - Cannabis is regularly known to improve the taste of foods.
- Bodily pressures - This can be described a subtle or distinct pressure felt behind one's eye(s).
- Bronchodilation[citation needed]
- Changes in felt gravity - At extremely high doses, many users report a feeling of being pulled backwards across vast distances (sometimes at powerful speeds). This sensation progressively increases in intensity and often eventually becomes unbearable if one leans backwards or lies down; however, it disappears altogether once the user sits up or leans forward.
- Increased heart rate[39] - Decreased blood pressure can result in an increased heart rate, although this varies depending on the user.
- Decreased blood pressure[39]
- Dizziness - Cannabis has the potential to cause dizziness at very high doses. However, this effect is far more inconsistent than with substances such as alcohol.
- Dehydration
- Dry mouth[39] - This is known colloquially as "cotton mouth" in popular American and United Kingdom culture. Edible forms of cannabis can make this effect feel much more intense and uncomfortable.
- Increased perspiration - This effect is experienced almost exclusively with the convection of solvent extracted hash oil and appears almost immediately upon exhalation. This is likely due to the high THC concentration and a relatively rapid onset that can result in a significant decrease in blood pressure, often causing the user to sweat.
- Insomnia - Chronic intake is associated with insomnia.[44]
- Motor control loss - This substance causes a partial to moderate suppression of motor control which intensifies proportional to dose, but rarely results in a complete inability to walk and perform basic movements.
- Muscle relaxation
- Muscle spasms - This effect is usually very subtle and is more likely to occur at high doses.
- Nausea - At heavy dosages and overdoses, cannabis can be nauseating. This usually passes after the first 30 or 40 minutes of the intoxication and tends to transition later into nausea suppression.
- Nausea suppression - Cannabis is effective for suppressing nausea induced by both general illness and substances. It is considered an effective treatment for chemotherapy-induced nausea and vomiting (CINV)[26] and is a reasonable option in those who do not improve following preferential treatment.[45]
- Pain relief - This substance has been reported as useful for treating certain headaches and chronic pain, including pain caused by neuropathy and possibly fibromyalgia and rheumatoid arthritis.[46][47]
- Perception of bodily lightness or Perception of bodily heaviness - Depending on the specific strain of cannabis, one can find themselves with a body which can feel either physically heavier or lighter than it usually would in a style that is entirely dependent upon dose or tolerance of the individual.
- Physical euphoria - This rarely exceeds mild to moderate levels of intensity, and although this effect may be present for many users there are also a number of individuals who report experiencing no euphoria at all. For some, this effect is notably more prominent with edible forms of cannabis.
- Red eye - Marijuana induces corneal vasodilation (so called red eye) and a reduction of intraocular pressure (IOP).[48] Naphazoline eye drops relieve red eyes.
- Seizure suppression - There are many anecdotal reports of the successful treatment of seizures in epilepsy with the use of low THC/high CBD marijuana.[49][50][51] However, there is not enough scientific evidence to draw conclusions about its safety or efficacy. Studies in animals have found that cannabidiol,[52][53] tetrahydrocannabivarin (THCV),[54] and other cannabinoids have anticonvulsant properties.[55]
- Tactile enhancement
- Vasodilation - THC decreases blood pressure which dilates the blood vessels and increases blood flow throughout the body. The arteries in the eyeball expand from the decreased blood pressure. These enlarged arteries often produce a bloodshot red eye effect and is the basis for its effectiveness at treating glaucoma.[56] Studies have shown cannabis (smoked or eaten) effectively lowers intraocular pressure by about 25%, as much as standard medications.[57]
- Sedation[39] - Cannabis may produce a mild sense of stimulation at low to moderate doses. Its effects are primarily sedating and can even be hypnotic. These relaxing properties are suppressed by consciously forcing oneself to engage in physical activities.
Visual effects 
-
Cannabis inconsistently induces visual and hallucinatory states at higher doses. These hallucinations are very mild and ill-defined compared to the effects of hallucinogens like psychedelics, dissociatives, and deliriants.
- Colour enhancement - This effect is often faint, but has been known to increase in its likeness and/or appearance among "regular" users of psychedelics.
- Acuity suppression - THC is known to decrease intraocular pressure.[58] This can sometimes result in blurry vision for some people.[citation needed]
- Brightness alteration - THC has been shown to modulate the activity of cone cells in the eye. This can cause an increased sensitivity to light, causing one's vision to appear brighter than normal.
- Pattern recognition enhancement - This effect can occur at high doses
- Tracers - This effect can be seen at high doses and is generally quite mild. It generally does not extend past level 2.
- Geometry - Cannabis is capable of inconsistently inducing mild psychedelic geometry at extremely high doses within many users who also regularly use psychedelics. It is capable of inducing these in a visual style which seems to be an averaged out depiction of all the psychedelics one has used within the past. These rarely extend beyond level 4 and are considered to be mild, fine, small and zoomed out (but often well-defined).
- Internal hallucination - The internal hallucinations of cannabis are extremely variable in their appearance depending on the dosage, tolerance and the individual's brain chemistry. They are very inconsistent and for some even rare but can be described as being fainter in appearance when compared to traditional psychedelics and do not seem to be as regularly composed of visual geometry.
The most common way in which they manifest themselves is through hypnagogic scenarios. They are most common during high dosages in dark environments and can be comprehensively described through their variations as both lucid and delirious in believability, fixed in style, autonomous in controllability, equal in new experiences and memory replays in content and are primarily geometry-based in style.
- Peripheral information misinterpretation - This very inconsistent effect tends to be mild and fleeting in contrast to other more powerful psychoactive substances. This effect rarely occurs on cannabis alone but when it does it is often in high dosages and/or when the individual has a low tolerance. It is more likely to manifest itself in certain environments as opposed to others and is more likely to happen if one has used stronger substances recently, typically within the past 24 to 36 hours.
- Visual disconnection
Cognitive effects 
-
- Anxiety or Anxiety suppression
- Analysis enhancement - This effect is significantly less prominent and consistent than it is with serotonergic psychedelics and stimulants.
- Analysis suppression
- Conceptual thinking
- Cognitive euphoria - This effect is generally mild and usually only present during the onset and peak of intoxication
- Creativity enhancement
- Delusion
- Depersonalization
- Derealization
- Dream suppression - It is commonly reported that regular cannabis use before sleep results in a complete absence of dreams. A day or two of abstaining from cannabis results in an intensification of dreams for a short period of time.
This claim is supported through studies that demonstrate that measurably reduced eye movement activity and REM states occur when one falls asleep in the THC condition. This state is strongly associated with dreaming. The same study also reported a REM rebound effect; there is more REM activity during the withdrawal from THC.[59]
- Decreased libido and Increased libido - Although cannabis is commonly reported to increase sexual desire and heighten its pleasure it has also been reported to decrease one's libido as well.
The decrease in libido typically only occurs during the onset of the intoxication whilst the increase in libido commonly occurs during the offset or after the peak effects. However, these components are inconsistent and it is possible for one of these effects to occur without the other.
- Emotion enhancement - The most prominent cognitive component of the cannabis experience is the way in which it enhances the emotions one is already feeling proportional to dose. This can result in euphoria, extreme laughter, and increased immersion within tasks and activities or it can result in anxiety and paranoia depending on the user's current state of mind.
- Feelings of impending doom - This occurs in high doses, it consists of extreme anxiety and paranoia. It can be compared to a mild "bad trip" on psychedelics.
- Focus suppression and Focus enhancement - This can depend on the user, dose, method or the strain of cannabis used. Higher doses tend to cause focus suppression while lower doses can increase one's focus.
- Immersion enhancement
- Increased music appreciation
- Increased sense of humor
- Laughter fits - Cannabis can often cause spurts of laughter for little, to no reason. This is often where the term "giggles" comes from when people are high off cannabis [60].
- Memory suppression - Cannabis is known to suppress short-term memory due to inhibition of glutamate neurotransmission in the hippocampus. This effect primarily effects short-term memory, making ego death or long-term memory suppression very unlikely.
- Mindfulness
- Motivation suppression[61]
- Novelty enhancement - Relatively consistent, but not as pronounced as with psychedelics. This effect can become more noticeable and/or consistent if the individual regularly takes psychedelics.
- Paranoia - All cannabinoids are capable of inducing paranoia at high doses, with chronic administration, or when administered alongside psychedelics or stimulants.
- Personal meaning enhancement
- Psychosis - The prolonged usage of THC may increase one's disposition to psychosis[62], particularly in vulnerable individuals with risk factors for psychotic illnesses (like a past or family history of schizophrenia).[63]
- Sleepiness - This effect depends mostly on dose and/or strain of the plant and is most prominent after the peak subsides.
- Suggestibility enhancement
- Thought connectivity - Cannabis can often cause many wandering thoughts and ideas at most doses.
- Thought deceleration
- Time distortion - Cannabis has been commonly reported to alter one's sense of time. The distortion that occurs is generally mild, and is most commonly reported to be in the form of time expansion.
Auditory effects 
-
- Enhancements
- Distortions - These are usually only present at extremely high doses.
Multi-sensory effects 
-
- Synaesthesia - This is a very rare and typically non-reproducible effect. It is particularly mild when compared to the states capable of being produced by other hallucinogens, particularly serotonergic psychedelics. Increasing the dosage can increase the likelihood for this effect to occur, but otherwise only seems to be possible among those who are already predisposed to synaesthetic states.
Combination effects
- Psychedelics - Cannabis strongly intensifies the sensory and cognitive effects of all psychedelics. Extreme caution is advised when combining these substances as this can significantly increase the chances of a negative psychological reaction like anxiety, confusion and psychosis. Users are advised to start off with only a fraction of their usual cannabis dose and take long breaks between hits. Many users report that cannabis is effective at briefly recreating the peak of the experience if consumed during the come down phase.
- Dissociatives - Cannabis enhances the cognitive, visual and general hallucinatory effects of dissociatives. Dissociative-induced holes, spaces, and voids and internal hallucinations become more vivid and intense on cannabis. These effects correspond with an increased risk of confusion, delusions, and psychosis.
- Depressants - Depressants such as benzodiazepines or opioids reduce the hallucinogenic aspects of the cannabis high. Instead, the focus shifts to bodily sensations, such as muscle relaxation, sedation, information processing suppression, and anxiety suppression.
- Alcohol - When used with alcohol, cannabis often creates feelings of extreme nausea, double vision, dizziness and changes in gravity. It is generally recommended that people take the cannabis before drinking and not the other way around as this is reported to induce these effects less readily.
- Stimulants - Cannabis tends to increase the thought accelerating, immersion enhancing and euphoric effects of stimulants, particularly as it relates to one's appreciation of music and sexual pleasure. This combination should be used with caution, however, as it can easily induce states of anxiety, paranoia, confusion, delusions, and psychosis.
Experience reports
Anecdotal reports which describe the effects of this compound within our experience index include:
- Experience: 100ug ALD-52 - Nice weekend trip
- Experience: 2.5 hits - Cannabis Sativa? - Smoked - Cognitive Experiment
- Experience: 25mg 50% DMT Changa + Cannabis (Smoked - Bong) - Insights into my consciousness
- Experience: 25ug ALD-52 - Untitled
- Experience: 2g Psilocybe cubensis (Lemon Tek) + 0.25mg Cannabis (Bong) - Passing through The Doors to the Eternal Summer
- Experience: 450mg DXM + THC - A shallow dive into the 3rd plateau
- Experience: Cannabis Hybrid (moderate dose, smoked and vaporized)
- Experience:1000 Morning Glory seeds - Rediscovering the Self
- Experience:175mg Mirtazapine and 1g D8 Cannabis - Bugs, Lizards and Continuity
- Experience:17mg 3-MeO-PCP & Cannabis oil - Terrifying confusion
- Experience:2 hits of LSD + weed - Mindfuck
- Experience:3 bowls of cannabis indica - I wrote down unintelligible gibberish
- Experience:3.5g psilocybe cubensis - Relinquishing of Material Chains/Fear and Desolation
- Experience:300mg Cannabis Unity
- Experience:300mg DXM + 25mg DMT + Cannabis - A crazy night
- Experience:337mg DMT fumarate - A Day With DMT
- Experience:400ug LSD + weed + nitrous -- Fundamental insights into the universe
- Experience:400µg LSD + 7.9g cannabis - Pure Energy
- Experience:40mg - Brothermind and the Forest's Hand
- Experience:5 tabs LSD + cannabis + nitrous - A lover's ego death
- Experience:A combination of DOC, 5-MAPB, 5-MeO-DMT, ETH-LAD, Cannabis, Pentedrone
- Experience:An Excessive Amount - N,N DMT / Marijuana - Stuck Inside an Egg
- Experience:An experiement combining mangoes and cannabis
- Experience:Cannabis (50-75mg, Edible) - OEV's
- Experience:Cannabis (Smoked) - Memes at School
- Experience:Cannabis 5 Hits - Awesome in Retrospect
- Experience:Cannabis, Ecstasy (3 brownies, 1 pill, Oral) My happy friends Shadow People
- Experience:Citalopram 10 mg and Cannabis 7 hits
- Experience:Creative Bliss
- Experience:DXM (340 mg) + DMT (30 mg, smoked) + Cannabis - Amazing Synergy
- Experience:First 105μg LSD - Unlocking The Door
- Experience:Kratom + Phenibut + Cannabis - Warm Bliss
- Experience:LSD (150µg) + Cannabis - 150µg lsd and a shitload of weed
- Experience:LSD (220 ug) and Cannabis - Tripping at home
- Experience:MDMA (100 mg) + Cannabis - Trip Report
- Experience:MDMA (750mg, Oral) - Finally Free
- Experience:Marijuana Withdrawal
- Experience:Meditation with cannabis - terminated ego loss
- Experience:Methamphetamine (20-40 mg insufflated) + cannabis - Hallucinatory Overdose
- Experience:Mushrooms and Snuff Films -- Trip Report (3.5 grams)
- Experience:Psilocybin or O-Acetylpsilocin (8000mg oral) - Don't you see? Don't you realize?
- Experience:Psychedelic Experience on Cannabis - Meeting Zeus
- Experience:Unknown dose - Supermarket dislocation and biking
Additional experience reports can be found here:
Dosage and preparation
THC
"Our results showed an overall increase in potency of illicit cannabis, from approximately 10% in 2009 to approximately 14% in 2019. These results are in agreement with other potency monitoring programs in several European countries."[64]
Math to calculate the quantity needed weed: Desired THC from divided by the THC strength of the strain. For example, if you want to smoke 3 mg (a common dose) from cannabis with 12% THC:
- 3 mg / 12% = 3/0.12 = 25 mg
Strains and forms
Strains
Sativa and indica are the two major types of cannabis plants which can mix together to create hybrid strains. Because each strain has its own balance of cannabinoids, each strain has its own range of effects on the body and mind, resulting in a wide range of medicinal benefits.
Indica plants typically grow short and wide compared to sativa plants which grow tall and thin. Indica plants are better suited for indoor growing because of their short growth and sativa plants are better suited for outdoor growing because some strains can reach over 25 ft. in height.
Marijuana strains range from pure sativas to pure indicas with hybrid strains consisting of both indica and sativa (for example, 30% indica – 70% sativa, 50% – 50% combinations, or 80% indica – 20% sativa).
Hypothetical phytocannabinoiod differences between C. indica and C. sativa
The effects of sativa may be used for a high, while indica may be used for its sedative effects. Both types are used as medical cannabis.
- Cannabinoid ratios: On average, Cannabis indica has higher levels of THC compared to CBD, whereas Cannabis sativa has lower levels of THC to CBD.[65] However, huge variability exists within either species. A 2015 study shows the average THC content of the most popular herbal cannabis products in the Netherlands has decreased slightly since 2005.[66]
- Terpene ratios: Sativa ancestry is associated with farnesene and [ergamotene, while Indica ancestry is associated with myrcene, elemene, and sesquiterpene alcohols.
Criticism
In 2022, studies found that plants identified as "indica" or "sativa" based on common methods of differentiation (e.g. plant height or leaf shape) are not, in fact, chemically distinguishable, with many identified as "sativa" having cannabinoid ratios predicted of "indica" plants and vice versa. The authors have concluded that the chemical makeup of cannabis plants cannot be reliably determined by simple inspection of the plants' physical characteristics and that the "indica" and "sativa" labels are not informative as to the cannabinoids (or other chemical components) delivered.[67][68]
Forms
Kief is a powder which can be sifted from the leaves and flowers of cannabis plants and either consumed in powder form or compressed to produce cakes of hashish.[71]
Hashish (also spelled hasheesh, hashisha, or simply hash) is a concentrated resin cake or ball produced from pressed kief. Hashish was the primary form of cannabis used in Europe in 2008. Herbal cannabis is more widely used in Northern America. Purities of confiscated hashish in Europe (2011) range between 4-15%. Between 2000 and 2005 the percentage of hashish in cannabis end product seizures was at 18%.[72]
Common usage
Consumption methods
Cannabis is consumed in many different ways:[76]
- Smoking typically involves inhaling vaporized cannabinoids ("smoke") from small pipes, bongs (portable versions of hookahs with water chamber), paper-wrapped joints, tobacco-leaf-wrapped blunts, and other items.[77]
- Vaporizers heat herbal cannabis to 165–190 °C (329–374 °F), causing the active ingredients to evaporate into a vapor without burning the plant material (the boiling point of THC is 157 °C (315 °F) at 760 mmHg pressure).[78]
- Cannabis tea contains relatively small concentrations of THC because THC is an oil (lipophilic) and is only slightly water-soluble (with a solubility of 2.8 mg per liter).[79] Cannabis tea is made by first adding a saturated fat to hot water (e.g., cream or any milk except skim) with a small amount of cannabis.[80]
- Edibles are cannabis added as an ingredient to one of a variety of foods.
- Sublingual/buccal consumption typically involves the absorption of cannabinoids through the membranes inside the mouth (usually through a candy or tincture).
- Tinctures vary from edibles, usually only containing extracted (and potent) THC in liquid form. Tinctures can be taken sublingually, or orally.
- Topical consumption typically involves the use of either a cream or lip balm containing cannabinoids absorbed through the skin.
Preparation methods
Preparation methods for this compound within our tutorial index include:
- Butane hash oil extraction
- Isopropyl extraction of crude cannabis oil
- Cannabis butter
- Cannabis cookies
- Green dragon tek
Medical use
Cannabis is an emerging treatment option for those suffering from many serious diseases, including cancer. Due to its pain relieving, nausea suppressing effects, cannabis can be useful for those undergoing radiation therapy and chemotherapy.[81] Oral doses of cannabis are more effective in reducing nausea and vomiting[82].
In addition to the anti-nausea effects, the appetite enhancement effects of cannabis can combine with the antiemetic effects and make it more likely that the patient will gain or maintain weight through cancer treatment.[83]
Toxicity and harm potential
Cannabis is common, and its tolerance is moderate, so intoxication can occur frequently. Frequent use of cannabis with more than 10% THC increased the risk of developing a psychotic disorder. 5% THC provides pain relief as well as intoxication.[84] We recommend you to dilute your cannabis product (see below). Analysis of data from 901 patients showed that the use of high-potency cannabis (THC content ≥10%) was associated with a modestly increased risk of developing a psychotic disorder compared to never using cannabis.[85] Street cannabis has an average THC content of 12%,[86] and medical cannabis products have more than 10% THC.[84] We recommend you to weigh and dilute cannabis buds, and hashish, with 3 times more, and 10 times more hemp respectively. Avoid mixing with tobacco to avoid nicotine: Stimulants should be used with caution in combination with [quasi-]psychedelics including cannabis. |

Despite its reputation for being a benign substance, it is important to be aware that cannabis use is associated with distinct risks. Acute adverse effects include anxiety, hyperemesis syndrome, impaired coordination and judgment, suicidal ideations/tendencies, and psychotic symptoms.
It is strongly advised to use harm reduction practices if using this substance.
Cannabinoid hyperemesis syndrome (CHS) is recurrent nausea, vomiting, and stomach cramp that sometimes occurs due to prolonged, high-dose cannabis use.[89][90]
Cannabis arteritis (CA) is a very rare peripheral vascular disease similar to Buerger's disease.[91]
Cannabis use during brain development (including during pregnancy and adolescence) has been shown to interfere with a variety of neurobiological systems. Meta-analysis following ~5 weeks of abstinence reveals lasting changes in the central executive and default mode networks, which are involved in attention and working memory. The extent of these changes as risk factors is not entirely clear.[92]
Suicidality
A NIH study found that suicide risk is higher with marijuana users than non-users. [93]
On the other hand, the largest study as of 2018 in association with cannabis use and the risk of suicide, there was no found evidence between the two. This study shows that it is unlikely a risk factor for suicide, either directly or as a consequence of use. [94]
Not only that, but another study studied the association between cannabis and suicidality also has correlation.[95]
The main takeaway from these studies and more is that while suicide risk may be higher with people who use cannabis, cannabis is unlikely the cause or an additional significant factor.
Psychosis risk
The prolonged usage of THC and other cannabinoids may increase one's disposition to mental illness and psychosis,[62] particularly in vulnerable individuals with risk factors for psychotic illnesses (like a past or family history of schizophrenia).[96][97][63]
Individuals with a personal or family history of mental illness, particularly psychotic disorders like schizophrenia, should not use cannabis without the advice of a qualified mental health practitioner.
Trauma
use and trauma are linked, with trauma playing a role in encouraging both the use and potential misuse of cannabis.[98] Conversely, cannabis use has been associated with the intensity of trauma and PTSD symptoms.[99][100] While evidence of efficacious use of cannabis is growing in novelty, it is not currently recommended.[101][102]
Lethal dosage
No fatal overdoses associated with cannabis use have been reported as of 2010.[103] A review published in the British Journal of Psychiatry in February 2001 said that "no deaths directly due to acute cannabis use have ever been reported."[104]
THC, the principal psychoactive constituent of the cannabis plant, has extremely low physiological toxicity and the amount that can enter the body through the consumption of cannabis plants poses no threat of death. In lab animal tests, scientists have had much difficulty administering a dose of THC that is high enough to be lethal. The dose of THC needed to kill 50% of tested rodents is very high,[105] 2.594 mol/kg, about 815.7 grams of THC per kilogram of body weight,[106] and human deaths from overdose are unheard of.[107]
At present, it is estimated that the LD50 of cannabis is around 1:20,000 or 1:40,000. This means that, in order to induce death, a cannabis smoker would have to consume 20,000 to 40,000 times as much cannabis as is contained in one cannabis cigarette. A user would theoretically have to smoke nearly 1,500 pounds of cannabis within about 15 minutes to induce a lethal response.
It is worth noting that the rare condition Cannabinoid Hyperemesis Syndrome (CHS) can cause ongoing nausea, vomiting and severe dehydration which can lead to renal failure[108] and in the worst case this can lead to death.[109]
Dependence and abuse potential
Cannabis is moderately habit-forming. Research has shown the overall dependence potential for cannabis to be less than that for caffeine, tobacco, alcohol, cocaine or heroin, but higher than that for psilocybin, mescaline, or LSD.[110]
Dependence on cannabis is more common amongst heavy users. Cannabis use can lead to increased tolerance[26][111] and withdrawal symptoms upon stopping usage.[34][112] Prolonged cannabis usage requires the user to consume higher doses of the substance to achieve a common desirable effect, and reinforce the body's metabolic systems for synthesizing and eliminating it more efficiently.[113]
Tolerance to many of the effects of cannabis develops with prolonged and repeated use. This results in users having to administer increasingly large doses to achieve the same effects. After that, it takes about 1 - 2 weeks for the tolerance to be reduced to half and 2 - 3 weeks to be back at baseline (in the absence of further consumption). THC has been detected in heavy cannabis users after 77 days of drug abstinence.[114]
Cannabis exhibits cross-tolerance with all cannabinoids, meaning that all cannabinoids will have a reduced effect for a period of time upon using cannabis. The mechanisms that create this tolerance to THC are thought to involve changes in cannabinoid receptor function.
One study found that about 1 in 10 users of cannabis may develop dependence characterized by the occurrence of a withdrawal syndrome after abstinence. This withdrawal syndrome was found to peak 2-3 days after quitting and is mostly complete by 1 week; however, sleep disturbances and vivid dreams may persist for 2-3 weeks.[115]
Dangerous interactions
Warning: Many psychoactive substances that are reasonably safe to use on their own can suddenly become dangerous and even life-threatening when combined with certain other substances. The following list provides some known dangerous interactions (although it is not guaranteed to include all of them).
Always conduct independent research (e.g. Google, DuckDuckGo, PubMed) to ensure that a combination of two or more substances is safe to consume. Some of the listed interactions have been sourced from TripSit.
- 2C-T-x
- 2C-x
- 5-MeO-xxT
- Amphetamines - Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences
- aMT
- Cocaine - Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences
- DMT
- DOx
- Lithium - Lithium is commonly prescribed in the treatment of bipolar disorder; however, there is a large body of anecdotal evidence that suggests taking it with cannabinoids can significantly increase the risk of psychosis and seizures. As a result, this combination should be strictly avoided.
- LSD
- Mescaline
- Mushrooms
- 25x-NBOMe
Legal status
For table of countries, see Wikipedia's global cannabis legalization table.
United Nations
The legality of cannabis for medical and recreational use varies by country, in terms of its possession, distribution, and cultivation, and (in regards to medical) how it can be consumed and what medical conditions it can be used for. These policies in most countries are regulated by the United Nations Single Convention on Narcotic Drugs that was ratified in 1961, along with the 1971 Convention on Psychotropic Substances and the 1988 Convention against Illicit Traffic in Narcotic Drugs and Psychotropic Substances.[116][99]
Rescheduling proposals
The World Health Organization (WHO) is calling for whole-plant marijuana, as well as cannabis resin, to be removed from Schedule IV—the most restrictive category of a 1961 drug convention signed by countries from around the world.[117]
See also
External links
Further reading
References
- ↑ Definition of THC
- ↑ Definition of Marijuana
- ↑ 3.0 3.1 Definition of Weed
- ↑ 4.0 4.1 Definition of POT
- ↑ 5.0 5.1 Definition of Grass
- ↑ 6.0 6.1 Definition of HEMP
- ↑ Definition of Zaza
- ↑ Definition of Kush
- ↑ 9.0 9.1 Erowid Cannabis Vault : Legal Status
- ↑ 10.0 10.1 WDR-2010
- ↑ Russo, E. B. (5 September 2013). Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Routledge. ISBN 9781136614934.
- ↑ El-Alfy, A. T., Ivey, K., Robinson, K., Ahmed, S., Radwan, M., Slade, D., Khan, I., ElSohly, M., Ross, S. (June 2010). "Antidepressant-like effect of Δ9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L". Pharmacology, biochemistry, and behavior. 95 (4): 434–442. doi:10.1016/j.pbb.2010.03.004. ISSN 0091-3057.
- ↑ Fusar-Poli, P., Crippa, J. A., Bhattacharyya, S., Borgwardt, S. J., Allen, P., Martin-Santos, R., Seal, M., Surguladze, S. A., O’Carrol, C., Atakan, Z., Zuardi, A. W., McGuire, P. K. (1 January 2009). "Distinct Effects of Δ9-Tetrahydrocannabinol and Cannabidiol on Neural Activation During Emotional Processing". Archives of General Psychiatry. 66 (1): 95. doi:10.1001/archgenpsychiatry.2008.519. ISSN 0003-990X.
- ↑ Booth, M. (30 September 2011). Cannabis: A History. Random House. ISBN 9781409084891.
- ↑ Clarke, P. B. (1986). Black paradise: the Rastafarian movement. New Religious Movements Series. Aquarian Pr. ISBN 9780850304282.
- ↑ Kevin Hill, MD, and MD Michael Hsu. “Cognitive Effects in Midlife of Long-Term Cannabis Use.” Harvard Health, 14 June 2022, https://www.health.harvard.edu/blog/cognitive-effects-of-long-term-cannabis-use-in-midlife-202206142760.
- ↑ ElSohly, M. A., ed. (2007). Marijuana and the cannabinoids. Forensic science and medicine. Humana Press. ISBN 9781588294562.
- ↑ http://www.unodc.org/pdf/WDR_2006/wdr2006_chap2_biggest_market.pdf
- ↑ ElSohly, M. A., Mehmedic, Z., Foster, S., Gon, C., Chandra, S., Church, J. C. (1 April 2016). "Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States". Biological Psychiatry. 79 (7): 613–619. doi:10.1016/j.biopsych.2016.01.004. ISSN 0006-3223.
- ↑ ElSohly, M. A., Mehmedic, Z., Foster, S., Gon, C., Chandra, S., Church, J. C. (1 April 2016). "Changes in Cannabis Potency over the Last Two Decades (1995-2014) - Analysis of Current Data in the United States". Biological psychiatry. 79 (7): 613–619. doi:10.1016/j.biopsych.2016.01.004. ISSN 0006-3223.
- ↑ 21.0 21.1 "Online Etymology Dictionary". Etymonline.com. Retrieved 17 February 2011.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedwikimarijuanaword - ↑ 23.0 23.1 23.2 Ben Amar, M. (April 2006). "Cannabinoids in medicine: A review of their therapeutic potential". Journal of Ethnopharmacology. 105 (1–2): 1–25. doi:10.1016/j.jep.2006.02.001. ISSN 0378-8741.
- ↑ Downer, E. J., Campbell, V. A. (5 August 2009). "Phytocannabinoids, CNS cells and development: A dead issue?: Phytocannabinoids have neurotoxic properties". Drug and Alcohol Review. 29 (1): 91–98. doi:10.1111/j.1465-3362.2009.00102.x. ISSN 0959-5236.
- ↑ Burns, T. L., Ineck, J. R. (February 2006). "Cannabinoid Analgesia as a Potential New Therapeutic Option in the Treatment of Chronic Pain". Annals of Pharmacotherapy. 40 (2): 251–260. doi:10.1345/aph.1G217. ISSN 1060-0280.
- ↑ 26.0 26.1 26.2 Borgelt, L. M., Franson, K. L., Nussbaum, A. M., Wang, G. S. (February 2013). "The Pharmacologic and Clinical Effects of Medical Cannabis". Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 33 (2): 195–209. doi:10.1002/phar.1187. ISSN 0277-0008.
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ Cooke, Justin (25 January 2022). "How Are Cannabinoids Metabolized? (CBD, THC, CBG, THC-O, & More)". DailyCBD.
- ↑ https://pubs.acs.org/doi/10.1021/acs.chemrestox.2c00170
- ↑ https://www.erowid.org/library/books_online/future_synthetic/future_synthetic.shtml
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ Abioye, A; Ayodele, O; Marinkovic, A; Patidar, R; Akinwekomi, A; Sanyaolu, A (31 January 2020). "Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic benefit for the management of obesity and diabetes". Journal of cannabis research. 2 (1): 6. doi:10.1186/s42238-020-0016-7. PMC 7819335
 . PMID 33526143.
. PMID 33526143.
- ↑ 34.0 34.1 Gordon, A. J., Conley, J. W., Gordon, J. M. (14 November 2013). "Medical Consequences of Marijuana Use: A Review of Current Literature". Current Psychiatry Reports. 15 (12): 419. doi:10.1007/s11920-013-0419-7. ISSN 1535-1645.
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK564166/
- ↑ Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors
- ↑ Hejazi, N., Zhou, C., Oz, M., Sun, H., Ye, J. H., Zhang, L. (1 March 2006). "Δ9-Tetrahydrocannabinol and Endogenous Cannabinoid Anandamide Directly Potentiate the Function of Glycine Receptors". Molecular Pharmacology. 69 (3): 991–997. doi:10.1124/mol.105.019174. ISSN 0026-895X.
- ↑ Franklin, J. M., Carrasco, G. A. (March 2013). "Cannabinoid receptor agonists upregulate and enhance serotonin 2A (5-HT 2A ) receptor activity via ERK1/2 signaling". Synapse. 67 (3): 145–159. doi:10.1002/syn.21626. ISSN 0887-4476.
- ↑ 39.0 39.1 39.2 39.3 Robson, P. (2001). "Therapeutic aspects of cannabis and cannabinoids". The British Journal of Psychiatry. 178 (2): 107–115. doi:10.1192/bjp.178.2.107. ISSN 0007-1250.
- ↑ Mechoulam, Raphael; Parker, Linda A.; Gallily, Ruth (2002). "Cannabidiol: An Overview of Some Pharmacological Aspects". The Journal of Clinical Pharmacology. 42 (S1): 11S–19S. doi:10.1002/j.1552-4604.2002.tb05998.x. ISSN 0091-2700.
- ↑ Mechoulam, R., ed. (1986). Cannabinoids as therapeutic agents. CRC Press. ISBN 9780849357725.
- ↑ Investigating the Neuroendocrine and Behavioral Controls of Cannabis-Induced Feeding Behavior. JF Davis, PQ Choi, J Kunze, P Wahl, Washington State University Pullman, WA, USA. Presented July 2018, Society for the Study of Ingestive Behavior, Bonita Springs, FL.
- ↑ An Overview Of Tetrahydrocannabivarin (THCV), 2013
- ↑ Wong, MM; Craun, EA; Bravo, AJ; Pearson, MR; Protective Strategies Study, Team. (August 2019). "Insomnia symptoms, cannabis protective behavioral strategies, and hazardous cannabis use among U.S. college students". Experimental and clinical psychopharmacology. 27 (4): 309–317. doi:10.1037/pha0000273. PMID 30907602.
- ↑ Ärzteblatt, D. Ä. G., Redaktion Deutsches, The Therapeutic Potential of Cannabis and Cannabinoids (23.07.2012)
- ↑ Martín-Sánchez, E., Furukawa, T. A., Taylor, J., Martin, J. L. R. (November 2009). "Systematic Review and Meta-analysis of Cannabis Treatment for Chronic Pain". Pain Medicine. 10 (8): 1353–1368. doi:10.1111/j.1526-4637.2009.00703.x. ISSN 1526-2375.
- ↑ Lynch, M. E., Campbell, F. (November 2011). "Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials: Cannabinoids for pain". British Journal of Clinical Pharmacology. 72 (5): 735–744. doi:10.1111/j.1365-2125.2011.03970.x. ISSN 0306-5251.
- ↑ Yazulla, S (September 2008). "Endocannabinoids in the retina: from marijuana to neuroprotection". Progress in retinal and eye research. 27 (5): 501–26. doi:10.1016/j.preteyeres.2008.07.002. PMID 18725316.
- ↑ Osborne, H. (2014), Charlotte Figi: The Girl Who is Changing Medical Marijuana Laws Across America
- ↑ On the frontier of medical pot to treat boy’s epilepsy, 2012
- ↑ Porter, B. E., Jacobson, C. (December 2013). "Report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy". Epilepsy & behavior : E&B. 29 (3): 574–577. doi:10.1016/j.yebeh.2013.08.037. ISSN 1525-5050.
- ↑ Jones, N. A., Hill, A. J., Smith, I., Bevan, S. A., Williams, C. M., Whalley, B. J., Stephens, G. J. (February 2010). "Cannabidiol displays antiepileptiform and antiseizure properties in vitro and in vivo". The Journal of Pharmacology and Experimental Therapeutics. 332 (2): 569–577. doi:10.1124/jpet.109.159145. ISSN 1521-0103.
- ↑ Turkanis, S. A., Smiley, K. A., Borys, H. K., Olsen, D. M., Karler, R. (August 1979). "An electrophysiological analysis of the anticonvulsant action of cannabidiol on limbic seizures in conscious rats". Epilepsia. 20 (4): 351–363. doi:10.1111/j.1528-1157.1979.tb04815.x. ISSN 0013-9580.
- ↑ Hill, A. J., Weston, S. E., Jones, N. A., Smith, I., Bevan, S. A., Williamson, E. M., Stephens, G. J., Williams, C. M., Whalley, B. J. (August 2010). "Δ9-Tetrahydrocannabivarin suppresses in vitro epileptiform and in vivo seizure activity in adult rats". Epilepsia. 51 (8): 1522–1532. doi:10.1111/j.1528-1167.2010.02523.x. ISSN 1528-1167.
- ↑ Wallace, R. (May 2004). "Cannabinoids: Defending the Epileptic Brain". Epilepsy Currents. 4 (3): 93–95. doi:10.1111/j.1535-7597.2004.43003.x. ISSN 1535-7597.
- ↑ Is Marijuana an Effective Treatment for Glaucoma? - Medical Marijuana - ProCon.org
- ↑ Cardiovascular Effects of Cannabis | http://www.idmu.co.uk/canncardio.htm
- ↑ Purnell, W. D., Gregg, J. M. (1 July 1975). "Delta(9)-tetrahydrocannabinol,, euphoria and intraocular pressure in man". Annals of ophthalmology. 7 (7): 921–923. ISSN 0003-4886.
- ↑ Feinberg, I., Jones, R., Walker, J. M., Cavness, C., March, J. (April 1975). "Effects of high dosage delta-9-tetrahydrocannabinol on sleep patterns in man". Clinical Pharmacology & Therapeutics. 17 (4): 458–466. doi:10.1002/cpt1975174458. ISSN 0009-9236.
- ↑ Laughter fits
- ↑ Lac, A; Luk, JW (February 2018). "Testing the Amotivational Syndrome: Marijuana Use Longitudinally Predicts Lower Self-Efficacy Even After Controlling for Demographics, Personality, and Alcohol and Cigarette Use". Prevention science : the official journal of the Society for Prevention Research. 19 (2): 117–126. doi:10.1007/s11121-017-0811-3. PMID 28620722.
- ↑ 62.0 62.1 Arseneault, L., Cannon, M., Witton, J., Murray, R. M. (February 2004). "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry. 184 (2): 110–117. doi:10.1192/bjp.184.2.110. ISSN 0007-1250.
- ↑ 63.0 63.1 Vearrier, D., Osterhoudt, K. C. (June 2010). "A Teenager With Agitation: Higher Than She Should Have Climbed". Pediatric Emergency Care. 26 (6): 462–465. doi:10.1097/PEC.0b013e3181e4f416. ISSN 0749-5161.
- ↑ https://pubmed.ncbi.nlm.nih.gov/33508497/
- ↑ Karl W. Hillig; Paul G. Mahlberg (2004). "A chemotaxonomic analysis of cannabinoid variation in Cannabis (Cannabaceae)". American Journal of Botany. 91 (6): 966–975. doi:10.3732/ajb.91.6.966
 . PMID 21653452.
. PMID 21653452.
- ↑ Niesink RJ, Rigter S, Koeter MW, Brunt TM (2015). "Potency trends of Δ9-tetrahydrocannabinol, cannabidiol and cannabinol in cannabis in the Netherlands: 2005-15". Addiction. 110 (12): 1941–50. doi:10.1111/add.13082. PMID 26234170.
- ↑ Smith, Christiana J.; Vergara, Daniela; Keegan, Brian; Jikomes, Nick (2022). "The phytochemical diversity of commercial Cannabis in the United States". PLOS ONE. 17 (5): –0267498. Bibcode:2022PLoSO..1767498S. doi:10.1371/journal.pone.0267498
 . ISSN 1932-6203. PMC 9119530
. ISSN 1932-6203. PMC 9119530  Check
Check |pmc=value (help). PMID 35588111. - ↑ Murovec, Jana; Eržen, Jan Jurij; Flajšman, Marko; Vodnik, Dominik (2022). "Analysis of Morphological Traits, Cannabinoid Profiles, THCAS Gene Sequences, and Photosynthesis in Wide and Narrow Leaflet High-Cannabidiol Breeding Populations of Medical Cannabis". Frontiers in Plant Science. 13: 786161. doi:10.3389/fpls.2022.786161
 . ISSN 1664-462X. PMC 8907982
. ISSN 1664-462X. PMC 8907982  Check
Check |pmc=value (help). PMID 35283868. - ↑ Madrigal, A., High Times in Ag Science: Marijuana More Potent Than Ever
- ↑ Definition of marijuana, Dictionary.com
- ↑ Kief, Cannabis Culture, 2014
- ↑ EMCDDA (2008). "A cannabis reader: global issues and local experiences". Monograph Series. 8 (1). European Monitoring Centre for Drugs and Drug Addiction, Lisbon, doi:10.2810/13807
- ↑ "Section 1 THC Chemistry" (PDF).
- ↑ http://books.google.co.uk/books?id=x9Z1QZ5NIEIC&pg=PA78&redir_esc=y
- ↑ Gloss, D (October 2015). "An Overview of Products and Bias in Research". Neurotherapeutics. 12 (4): 731–4. doi:10.1007/s13311-015-0370-x. PMC 4604179
 . PMID 26202343.
. PMID 26202343.
- ↑ Golub, A. (6 December 2012). The Cultural/Subcultural Contexts of Marijuana Use at the Turn of the Twenty-First Century. Routledge. ISBN 9781136446276.
- ↑ Tasman, A., Kay, J., Lieberman, J. A., First, M. B., Maj, M. (11 October 2011). Psychiatry. John Wiley & Sons. ISBN 9781119965404.
- ↑ McPartland, J. M., Russo, E. B. (June 2001). "Cannabis and Cannabis Extracts: Greater Than the Sum of Their Parts?". Journal of Cannabis Therapeutics. 1 (3–4): 103–132. doi:10.1300/J175v01n03_08. ISSN 1529-9775.
- ↑ Dronabinol | http://chem.sis.nlm.nih.gov/chemidplus/rn/1972-08-3
- ↑ Gieringer, D. H., Rosenthal, E. (2008). Marijuana Medical Handbook: Practical Guide to Therapeutic Uses of Marijuana. Ed Rosenthal. ISBN 9780932551863.
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2005/018651s021lbl.pdf
- ↑ Sallan, S. E., Zinberg, N. E., Frei, E. I. (2010), Antiemetic Effect of Delta-9-Tetrahydrocannabinol in Patients Receiving Cancer Chemotherapy
- ↑ American College of Physicians. Supporting Research into the Therapeutic Role of Marijuana. Philadelphia: American College of Physicians; 2008: Position Paper. (Available from American College of Physicians, 190 N. Independence Mall West, Philadelphia, PA19106.) https://www.acponline.org/system/files/documents/advocacy/current_policy_papers/assets/medmarijuana.pdf
- ↑ 84.0 84.1 https://www.europeanpharmaceuticalreview.com/news/115909/over-90-percent-of-medical-marijuana-in-us-contains-high-levels-of-thc-study-finds/
- ↑ https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(19)30048-3/fulltext
- ↑ https://pubmed.ncbi.nlm.nih.gov/33508497/
- ↑ Nutt DJ, King LA, Phillips LD (November 2010). "Drug harms in the UK: a multicriteria decision analysis". Lancet. 376 (9752): 1558–1565. CiteSeerX 10.1.1.690.1283
 . doi:10.1016/S0140-6736(10)61462-6. PMID 21036393. Unknown parameter
. doi:10.1016/S0140-6736(10)61462-6. PMID 21036393. Unknown parameter |s2cid=ignored (help) - ↑ Nutt, D., King, L. A., Saulsbury, W., Blakemore, C. (24 March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". The Lancet. 369 (9566): 1047–1053. doi:10.1016/S0140-6736(07)60464-4. ISSN 0140-6736.
- ↑ Sorensen, Cecilia J.; DeSanto, Kristen; Borgelt, Laura; Phillips, Kristina T.; Monte, Andrew A. (20 December 2016). "Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment—a Systematic Review". Journal of Medical Toxicology. 13 (1): 71–87. doi:10.1007/s13181-016-0595-z. PMC 5330965
 . PMID 28000146.
. PMID 28000146.
- ↑ DeVuono, Marieka; Parker, Linda (2020). "Cannabinoid Hyperemesis Syndrome: A Review of Potential Mechanisms". Cannabis and Cannabinoid Research. 5: 132–144. doi:10.1089/can.2019.0059.
- ↑ El Omri, N; Eljaoudi, R; Mekouar, F; Jira, M; Sekkach, Y; Amezyane, T; Ghafir, D (2017). "Cannabis arteritis". The Pan African medical journal. 26: 53. doi:10.11604/pamj.2017.26.53.11694. PMID 28451030.
- ↑ Hurd, Yasmin L., et al. “Cannabis and the Developing Brain: Insights into Its Long-Lasting Effects.” Journal of Neuroscience, Society for Neuroscience, 16 Oct. 2019, https://www.jneurosci.org/content/39/42/8250.
- ↑ https://www.nih.gov/news-events/news-releases/canSuicidality
- ↑ Price, C., Hemmingsson, T., Lewis, G., Zammit, S., Allebeck, P. (December 2009). "Cannabis and suicide: longitudinal study". The British Journal of Psychiatry. 195 (6): 492–497. doi:10.1192/bjp.bp.109.065227. ISSN 0007-1250.
- ↑ Borges, G., Bagge, C. L., Orozco, R. (1 May 2016). "A literature review and meta-analyses of cannabis use and suicidality". Journal of Affective Disorders. 195: 63–74. doi:10.1016/j.jad.2016.02.007. ISSN 0165-0327.
- ↑ Every-Palmer, S. (September 2011). "Synthetic cannabinoid JWH-018 and psychosis: An explorative study". Drug and Alcohol Dependence. 117 (2–3): 152–157. doi:10.1016/j.drugalcdep.2011.01.012. ISSN 0376-8716.
- ↑ Schneir, A. B., Cullen, J., Ly, B. T. (1 March 2011). ""Spice" Girls: Synthetic Cannabinoid Intoxication". The Journal of Emergency Medicine. 40 (3): 296–299. doi:10.1016/j.jemermed.2010.10.014. ISSN 0736-4679.
- ↑ Hyman SM, Sinha R (June 2009). "Stress-related factors in cannabis use and misuse: implications for prevention and treatment". Journal of Substance Abuse Treatment. 36 (4): 400–13. doi:10.1016/j.jsat.2008.08.005. PMC 2696937
 . PMID 19004601.
. PMID 19004601.
- ↑ 99.0 99.1 Bonn-Miller MO, Vujanovic AA, Feldner MT, Bernstein A, Zvolensky MJ (August 2007). "Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users". Journal of Traumatic Stress. 20 (4): 577–86. doi:10.1002/jts.20243. PMID 17721963. Cite error: Invalid
<ref>tag; name ":0" defined multiple times with different content - ↑ Kevorkian S, Bonn-Miller MO, Belendiuk K, Carney DM, Roberson-Nay R, Berenz EC (September 2015). "Associations among trauma, posttraumatic stress disorder, cannabis use, and cannabis use disorder in a nationally representative epidemiologic sample". Psychology of Addictive Behaviors. 29 (3): 633–8. doi:10.1037/adb0000110. PMC 4699174
 . PMID 26415060.
. PMID 26415060.
- ↑ Black N, Stockings E, Campbell G, Tran LT, Zagic D, Hall WD, et al. (December 2019). "Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis". The Lancet. Psychiatry. 6 (12): 995–1010. doi:10.1016/s2215-0366(19)30401-8. PMC 6949116
 . PMID 31672337.
. PMID 31672337.
- ↑ Dagan Y, Yager J (August 2020). "Cannabis and Complex Posttraumatic Stress Disorder: A Narrative Review With Considerations of Benefits and Harms". The Journal of Nervous and Mental Disease. 208 (8): 619–627. doi:10.1097/nmd.0000000000001172. PMID 32433200. Unknown parameter
|s2cid=ignored (help) - ↑ Calabria, B., Degenhardt, L., Hall, W., Lynskey, M. (19 January 2010). "Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use: Adverse effects of cannabis use". Drug and Alcohol Review. 29 (3): 318–330. doi:10.1111/j.1465-3362.2009.00149.x. ISSN 0959-5236.
- ↑ Ashton, C. H. (February 2001). "Pharmacology and effects of cannabis: A brief review". The British Journal of Psychiatry. 178 (2): 101–106. doi:10.1192/bjp.178.2.101. ISSN 0007-1250.
- ↑ Hall, W., Solowij, N. (14 November 1998). "Adverse effects of cannabis". The Lancet. 352 (9140): 1611–1616. doi:10.1016/S0140-6736(98)05021-1. ISSN 0140-6736.
- ↑ https://www.drugbank.ca/drugs/DB00470
- ↑ Kochanowski, M., Kała, M. (2005). "Tetrahydrocannabinols in clinical and forensic toxicology". Przeglad Lekarski. 62 (6): 576–580. ISSN 0033-2240.
- ↑ Galli, J. A., Sawaya, R. A., Friedenberg, F. K. (December 2011). "Cannabinoid Hyperemesis Syndrome". Current drug abuse reviews. 4 (4): 241–249. ISSN 1874-4737.
- ↑ Nourbakhsh, M., Miller, A., Gofton, J., Jones, G., Adeagbo, B. (January 2019). "Cannabinoid Hyperemesis Syndrome: Reports of Fatal Cases". Journal of Forensic Sciences. 64 (1): 270–274. doi:10.1111/1556-4029.13819. ISSN 1556-4029.
- ↑ Lopez-Quintero, C., Cobos, J. P. de los, Hasin, D. S., Okuda, M., Wang, S., Grant, B. F., Blanco, C. (1 May 2011). "Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)". Drug and alcohol dependence. 115 (1–2): 120–130. doi:10.1016/j.drugalcdep.2010.11.004. ISSN 0376-8716.
- ↑ Sewell, R. A., Poling, J., Sofuoglu, M. (January 2009). "The Effect of Cannabis Compared with Alcohol on Driving". American Journal on Addictions. 18 (3): 185–193. doi:10.1080/10550490902786934. ISSN 1055-0496.
- ↑ Lichtman, A. H., Martin, B. R. (2005). "Cannabinoid tolerance and dependence". Handbook of Experimental Pharmacology (168): 691–717. doi:10.1007/3-540-26573-2_24. ISSN 0171-2004.
- ↑ Watson, S. J. (1 June 2000). "Marijuana and Medicine: Assessing the Science Base: A Summary of the 1999 Institute of Medicine Report". Archives of General Psychiatry. 57 (6): 547–552. doi:10.1001/archpsyc.57.6.547. ISSN 0003-990X.
- ↑ Ellis, G. M., Mann, M. A., Judson, B. A., Schramm, N. T., Tashchian, A. (November 1985). "Excretion patterns of cannabinoid metabolites after last use in a group of chronic users". Clinical Pharmacology and Therapeutics. 38 (5): 572–578. doi:10.1038/clpt.1985.226. ISSN 0009-9236.
- ↑ Winstock, A. R., Ford, C., Witton, J. (1 April 2010). "Assessment and management of cannabis use disorders in primary care". BMJ. 340 (apr01 1): c1571–c1571. doi:10.1136/bmj.c1571. ISSN 0959-8138.
- ↑ Habibi, Roojin; Hoffman, Steven J. (March 2018). "Legalizing Cannabis Violates the UN Drug Control Treaties, But Progressive Countries Like Canada Have Options". Ottawa Law Review. 49 (2). Retrieved 22 July 2018.
- ↑ Angell, T. (2019), World Health Organization Recommends Reclassifying Marijuana Under International Treaties