Talk:Delta-8-THC
This page has not been fully approved by the PsychonautWiki administrators. It may contain incorrect information, particularly with respect to dosage, duration, subjective effects, toxicity and other risks. It may also not meet PW style and grammar standards. |
| Summary sheet: Delta-8-THC |
For tips on how to properly format a substance article, please refer to this document: Content Style Guide - Substance
Delta-8-tetrahydrocannabinol (also known as Delta-8-THC and Δ-8-THC) is an isomer of Delta-9-tetrahydrocannabinol (also known as Delta-9-THC and Δ-9-THC). The effects of Delta-8-THC are nearly identical to those of Delta-9-THC, but slightly less potent.
History and culture
This History and culture section is a stub. As a result, it may contain incomplete or wrong information. You can help by expanding it. |
In 1941 Roger Adams and associates from the University of Illinois published the partial synthesis of Delta-8-THC.[1] By 1965 Raphael Mechoulam had completed the total synthesis of Delta-8-THC. Delta-8-THC didn't receive any further attention until 2018 when the Agriculture Improvement Act of 2018 was passed and a loophole was discovered in the act which allowed for the creation of Delta-8-THC "legally". Delta-8-THC use skyrocketed in many states where Marijuana remained illegal and in states where it was legal, consumption still increased as a result of the lack of regulation of Delta-8-THC.
Chemistry
This chemistry section is incomplete. You can help by adding to it. |
The only difference between Delta-8-THC and Delta-9-THC is the movement of a double bond.
Pharmacology
 |
This pharmacology section is incomplete. You can help by adding to it. |
The pharmacology of Delta-8-THC is nearly identical to that of Delta-9-THC. Delta-8-THC was shown to have a slower onset and a shorter duration. Onset varied from 30 to 90 minutes and peak effects were observed between 2-1/2 to 3-1/2 hours.[2]
|
Physical effects 
-
- Sedation[3] - Although certain strains of cannabis (e.g. sativas) produce a mild sense of stimulation at low to moderate doses, its effects are primarily sedating and can even be hypnotic. These relaxing properties are suppressed by consciously forcing oneself to engage in physical activities.
In terms of its stimulating effects, these subjective aspects of THC typically last 2-3 hours, whereas the half-life of CBD, which is more relaxing, is 9 hours.[4] Thus, the first dose of cannabis after a period of abstinence will tend to be far more stimulating than subsequent doses, which must compete with the relaxing effects of previous doses.
Because the relaxation both persists much longer and shares many of the same pathways as the stimulation, regular ingestion of THC also leads to increased tolerance to its stimulating effects, but not to its relaxing effects.[citation needed]
- Spontaneous bodily sensations - The "body high" of cannabis is extremely variable and depends entirely on the individual strain as well as dose and method of intake. In general, however, it can be described as a relatively pleasurable, sometimes warm, soft, intoxicating and all-encompassing sensation. At high dosages, it can cause some users to feel shaky or nerve-wracked.
- Appetite enhancement - The feeling of increased appetite following the use of cannabis has been documented for hundreds of years[5] and is known colloquially as "the munchies". Cannabis has been shown in recent studies to stimulate the release of the hormone ghrelin which is normally released by the stomach when empty as a signal for the brain to search for food.[6]
- Appetite suppression - This effect may present itself at the very beginning of the intoxication and is likely due mostly to the cannabinoid THCV.[7]
- Gustatory enhancement - Cannabis is regularly known to improve the taste of foods.
- Bodily pressures - This can be described a subtle or distinct pressure felt behind one's eye(s).
- Bronchodilation[citation needed]
- Changes in felt gravity - At extremely high doses, many users report a feeling of being pulled backwards across vast distances (sometimes at powerful speeds). This sensation progressively increases in intensity and often eventually becomes unbearable if one leans backwards or lies down; however, it disappears altogether once the user sits up or leans forward.
- Increased heart rate[3] - Decreased blood pressure can result in an increased heart rate, although this varies depending on the user.
- Decreased blood pressure[3]
- Dizziness - Cannabis has the potential to cause dizziness at very high doses. However, this effect is far more inconsistent than substances such as alcohol.
- Dehydration
- Dry mouth[3] - This is known colloquially as "cotton mouth" in popular American and United Kingdom culture. Edible forms of cannabis can make this effect feel much more intense and uncomfortable.
- Increased perspiration - This effect is experienced almost exclusively with the convection of solvent extracted hash oil and appears almost immediately upon exhalation. This is likely due to the high THC concentration and a relatively rapid onset that can result in a significant decrease in blood pressure, often causing the user to sweat.
- Insomnia - Chronic intake is associated with insomnia.[8]
- Motor control loss - This substance causes a partial to moderate suppression of motor control which intensifies proportional to dose, but rarely results in a complete inability to walk and perform basic movements.
- Muscle relaxation
- Muscle spasms - This effect is usually very subtle and is more likely to occur at high doses.
- Nausea - At heavy dosages and overdoses, cannabis can be nauseating. This usually passes after the first 30 or 40 minutes of the intoxication and tends to transition later into nausea suppression.
- Nausea suppression - Cannabis is effective for suppressing nausea induced by both general illness and substances. It is considered an effective treatment for chemotherapy-induced nausea and vomiting (CINV)[9] and is a reasonable option in those who do not improve following preferential treatment.[10]
- Pain relief - This substance has been reported as useful for treating certain headaches and chronic pain, including pain caused by neuropathy and possibly fibromyalgia and rheumatoid arthritis.[11][12]
- Perception of bodily lightness or Perception of bodily heaviness - Depending on the specific strain of cannabis, one can find themselves with a body which can feel either physically heavier or lighter than it usually would in a style that is entirely dependent upon dose or tolerance of the individual.
- Physical euphoria - This rarely exceeds mild to moderate levels of intensity, and although this effect may be present for many users there are also a number of individuals who report experiencing no euphoria at all. For some, this effect is notably more prominent with edible forms of cannabis.
- Red eye - Marijuana induces corneal vasodilation (so called red eye) and a reduction of intraocular pressure (IOP).[13] Naphazoline eye drops relieve red eyes.
- Seizure suppression - There are many anecdotal reports of the successful treatment of seizures in epilepsy with the use of low THC/high CBD marijuana.[14][15][16] However, there is not enough scientific evidence to draw conclusions about its safety or efficacy. Studies in animals have found that cannabidiol,[17][18] tetrahydrocannabivarin (THCV),[19] and other cannabinoids have anticonvulsant properties.[20]
- Tactile enhancement
- Vasodilation - THC decreases blood pressure which dilates the blood vessels and increases blood flow throughout the body. The arteries in the eyeball expand from the decreased blood pressure. These enlarged arteries often produce a bloodshot red eye effect and is the basis for its effectiveness at treating glaucoma.[21] Studies have shown cannabis (smoked or eaten) effectively lowers intraocular pressure by about 25%, as much as standard medications.[22]
- Sedation[3] - Although certain strains of cannabis (e.g. sativas) produce a mild sense of stimulation at low to moderate doses, its effects are primarily sedating and can even be hypnotic. These relaxing properties are suppressed by consciously forcing oneself to engage in physical activities.
Visual effects 
-
Cannabis inconsistently induces visual and hallucinatory states at higher doses. These hallucinations are very mild and ill-defined compared to the effects of hallucinogens like psychedelics, dissociatives, and deliriants.
- Colour enhancement - This effect is often faint, but has been known to increase in its likeness and/or appearance among "regular" users of psychedelics.
- Acuity suppression - THC is known to decrease intraocular pressure.[23] This can sometimes result in blurry vision for some people.[citation needed]
- Brightness alteration - THC has been shown to modulate the activity of cone cells in the eye. This can cause an increased sensitivity to light, causing one's vision to appear brighter than normal.
- Tracers - This effect can be seen at high doses and is generally quite mild. It generally does not extend past level 2.
- Geometry - Cannabis is capable of inconsistently inducing mild psychedelic geometry at extremely high doses within many users who also regularly use psychedelics. It is capable of inducing these in a visual style which seems to be an averaged out depiction of all the psychedelics one has used within the past. These rarely extend beyond level 4 and are considered to be mild, fine, small and zoomed out (but often well-defined).
- Internal hallucination - The internal hallucinations of cannabis are extremely variable in their appearance depending on the dosage, tolerance and the individual's brain chemistry. They are very inconsistent and for some even rare but can be described as being fainter in appearance when compared to traditional psychedelics and do not seem to be as regularly composed of visual geometry.
The most common way in which they manifest themselves is through hypnagogic scenarios. They are most common during high dosages in dark environments and can be comprehensively described through their variations as both lucid and delirious in believability, fixed in style, autonomous in controllability, equal in new experiences and memory replays in content and are primarily geometry-based in style.
- Peripheral information misinterpretation - This very inconsistent effect tends to be mild and fleeting in contrast to other more powerful psychoactive substances. This effect rarely occurs on cannabis alone but when it does it is often in high dosages and/or when the individual has a low tolerance. It is more likely to manifest itself in certain environments as opposed to others and is more likely to happen if one has used stronger substances recently, typically within the past 24 to 36 hours.
|
Cognitive effects 
-
- Amotivational syndrome[24]
- Anhedonia
- Anxiety or Anxiety suppression
- Analysis enhancement - This effect is significantly less prominent and consistent than it is with serotonergic psychedelics and stimulants.
- Analysis suppression
- Conceptual thinking
- Cognitive euphoria - This effect is generally mild and usually only present during the onset and peak of intoxication
- Creativity enhancement
- Delusion
- Depersonalization
- Derealization
- Dream suppression - It is commonly reported that regular cannabis use before sleep results in a complete absence of dreams. A day or two of abstaining from cannabis results in an intensification of dreams for a short period of time.
This claim is supported through studies that demonstrate that measurably reduced eye movement activity and REM states occur when one falls asleep in the THC condition. This state is strongly associated with dreaming. The same study also reported a REM rebound effect; there is more REM activity during the withdrawal from THC.[25]
- Decreased libido and Increased libido - Although cannabis is commonly reported to increase sexual desire and heighten its pleasure it has also been reported to decrease one's libido as well.
The decrease in libido typically only occurs during the onset of the intoxication whilst the increase in libido commonly occurs during the offset or after the peak effects. However, these components are inconsistent and it is possible for one of these effects to occur without the other.
- Emotion enhancement - The most prominent cognitive component of the cannabis experience is the way in which it enhances the emotions one is already feeling proportional to dose. This can result in euphoria, extreme laughter, and increased immersion within tasks and activities or it can result in anxiety and paranoia depending on the user's current state of mind.
- Feelings of impending doom - This occurs in high doses, it consists of extreme anxiety and paranoia. It can be compared to a mild "bad trip" on psychedelics.
- Focus suppression and Focus enhancement - This can depend on the user, dose, method or the strain of cannabis used. Higher doses tend to cause focus suppression while lower doses can increase one's focus.
- Immersion enhancement
- Increased music appreciation
- Increased sense of humor
- Laughter fits - Cannabis can often cause spurts of laughter for little, to no reason. This is often where the term "giggles" comes from when people are high off cannabis [26].
- Memory suppression - Cannabis is known to suppress short-term memory due to inhibition of glutamate neurotransmission in the hippocampus. This effect primarily effects short-term memory, making ego death or long-term memory suppression very unlikely.
- Mindfulness
- Novelty enhancement - Relatively consistent, but not as pronounced as with psychedelics. This effect can become more noticeable and/or consistent if the individual regularly takes psychedelics.
- Paranoia - All cannabinoids are capable of inducing paranoia at high doses, with chronic administration, or when administered alongside psychedelics or stimulants.
- Personal meaning enhancement
- Psychosis - The prolonged usage of THC may increase one's disposition to psychosis[27], particularly in vulnerable individuals with risk factors for psychotic illnesses (like a past or family history of schizophrenia).[28]
- Sleepiness - This effect depends mostly on dose and/or strain of the plant and is most prominent after the peak subsides.
- Suggestibility enhancement
- Thought connectivity - Cannabis can often cause many wandering thoughts and ideas at most doses.
- Thought deceleration
- Time distortion - Cannabis has been commonly reported to alter one's sense of time. The distortion that occurs is generally mild, and is most commonly reported to be in the form of time expansion.
Auditory effects 
-
- Enhancements
- Distortions - These are usually only present at extremely high doses.
Multi-sensory effects 
-
- Synaesthesia - This is a very rare and typically non-reproducible effect. It is particularly mild when compared to the states capable of being produced by other hallucinogens, particularly serotonergic psychedelics. Increasing the dosage can increase the likelihood for this effect to occur, but otherwise only seems to be possible among those who are already predisposed to synaesthetic states.
Combination effects
- Psychedelics - Cannabis strongly intensifies the sensory and cognitive effects of all psychedelics. Extreme caution is advised when combining these substances as this can significantly increase the chances of a negative psychological reaction like anxiety, confusion and psychosis. Users are advised to start off with only a fraction of their usual cannabis dose and take long breaks between hits. Many users report that cannabis is effective at briefly recreating the peak of the experience if consumed during the come down phase.
- Dissociatives - Cannabis enhances the cognitive, visual and general hallucinatory effects of dissociatives. Dissociative-induced holes, spaces, and voids and internal hallucinations become more vivid and intense on cannabis. These effects correspond with an increased risk of confusion, delusions, and psychosis.
- Depressants - Depressants such as benzodiazepines or opioids reduce the hallucinogenic aspects of the cannabis high. Instead, the focus shifts to bodily sensations, such as muscle relaxation, sedation, information processing suppression, and anxiety suppression.
- Alcohol - When used with alcohol, cannabis often creates feelings of extreme nausea, double vision, dizziness and changes in gravity. It is generally recommended that people take the cannabis before drinking and not the other way around as this is reported to induce these effects less readily.
- Stimulants - Cannabis tends to increase the thought accelerating, immersion enhancing and euphoric effects of stimulants, particularly as it relates to one's appreciation of music and sexual pleasure. This combination should be used with caution, however, as it can easily induce states of anxiety, paranoia, confusion, delusions, and psychosis.
Experience reports
There are currently 0 experience reports which describe the effects of this substance in our experience index.
Additional experience reports can be found here:
Toxicity and harm potential
 |
This toxicity and harm potential section is a stub. As a result, it may contain incomplete or even dangerously wrong information! You can help by expanding upon or correcting it. |
Despite its reputation for being a benign substance, it is important to be aware that cannabis use is associated with distinct risks. Acute adverse effects include anxiety, hyperemesis syndrome, impaired coordination and judgment, suicidal ideations/tendencies, and psychotic symptoms.
It is strongly advised to use harm reduction practices if using this substance.
Cannabinoid hyperemesis syndrome (CHS) is recurrent nausea, vomiting, and stomach cramp that sometimes occurs due to prolonged, high-dose cannabis use.[30][31]
Cannabis arteritis (CA) is a very rare peripheral vascular disease similar to Buerger's disease.[32]
Suicidality
A NIH study found that suicide risk is higher with marijuana users than non-users. [33]
On the other hand, the largest study as of 2018 in association with cannabis use and the risk of suicide, there was no found evidence between the two. This study shows that it is unlikely a risk factor for suicide, either directly or as a consequence of use. [34]
Not only that, but another study studied the association between cannabis and suicidality also has correlation.[35]
The main takeaway from these studies and more is that while suicide risk may be higher with people who use cannabis, cannabis is unlikely the cause or an additional significant factor.
Psychosis risk
The prolonged usage of THC and other cannabinoids may increase one's disposition to mental illness and psychosis,[36] particularly in vulnerable individuals with risk factors for psychotic illnesses (like a past or family history of schizophrenia).[37][38][39]
Individuals with a personal or family history of mental illness, particularly psychotic disorders like schizophrenia, should not use cannabis without the advice of a qualified mental health practitioner.
Lethal dosage
No fatal overdoses associated with cannabis use have been reported as of 2010.[40] A review published in the British Journal of Psychiatry in February 2001 said that "no deaths directly due to acute cannabis use have ever been reported."[41]
THC, the principal psychoactive constituent of the cannabis plant, has extremely low physiological toxicity and the amount that can enter the body through the consumption of cannabis plants poses no threat of death. In lab animal tests, scientists have had much difficulty administering a dose of THC that is high enough to be lethal. The dose of THC needed to kill 50% of tested rodents is very high,[42] 2.594 mol/kg, about 815.7 grams of THC per kilogram of body weight,[43] and human deaths from overdose are unheard of.[44]
At present, it is estimated that the LD50 of cannabis is around 1:20,000 or 1:40,000. This means that, in order to induce death, a cannabis smoker would have to consume 20,000 to 40,000 times as much cannabis as is contained in one cannabis cigarette. A user would theoretically have to smoke nearly 1,500 pounds of cannabis within about 15 minutes to induce a lethal response.
It is worth noting that the rare condition Cannabinoid Hyperemesis Syndrome (CHS) can cause ongoing nausea, vomiting and severe dehydration which can lead to renal failure[45] and in the worst case this can lead to death.[46]
Dependence and abuse potential
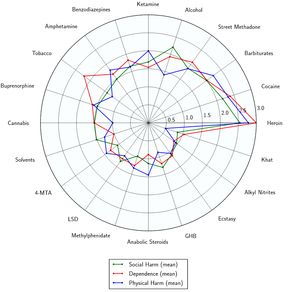
Cannabis is moderately habit-forming. Research has shown the overall dependence potential for cannabis to be less than that for caffeine, tobacco, alcohol, cocaine or heroin, but higher than that for psilocybin, mescaline, or LSD.[47]
Dependence on cannabis is more common amongst heavy users. Cannabis use can lead to increased tolerance[48][49] and withdrawal symptoms upon stopping usage.[50][51][52] Prolonged cannabis usage requires the user to consume higher doses of the substance to achieve a common desirable effect, and reinforce the body's metabolic systems for synthesizing and eliminating it more efficiently.[53]
Tolerance to many of the effects of cannabis develops with prolonged and repeated use. This results in users having to administer increasingly large doses to achieve the same effects. After that, it takes about 1 - 2 weeks for the tolerance to be reduced to half and 2 - 3 weeks to be back at baseline (in the absence of further consumption). THC has been detected in heavy cannabis users after 77 days of drug abstinence.[54]
Cannabis exhibits cross-tolerance with all cannabinoids, meaning that all cannabinoids will have a reduced effect for a period of time upon using cannabis. The mechanisms that create this tolerance to THC are thought to involve changes in cannabinoid receptor function.
One study found that about 1 in 10 users of cannabis may develop dependence characterized by the occurrence of a withdrawal syndrome after abstinence. This withdrawal syndrome was found to peak 2-3 days after quitting and is mostly complete by 1 week; however, sleep disturbances and vivid dreams may persist for 2-3 weeks.[55]
Dangerous interactions
Warning: Many psychoactive substances that are reasonably safe to use on their own can suddenly become dangerous and even life-threatening when combined with certain other substances. The following list provides some known dangerous interactions (although it is not guaranteed to include all of them).
Always conduct independent research (e.g. Google, DuckDuckGo, PubMed) to ensure that a combination of two or more substances is safe to consume. Some of the listed interactions have been sourced from TripSit.
- 2C-T-x
- 2C-x
- 5-MeO-xxT
- Amphetamines - Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences
- aMT
- Cocaine - Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences
- DMT
- DOx
- Lithium - Lithium is commonly prescribed in the treatment of bipolar disorder; however, there is a large body of anecdotal evidence that suggests taking it with cannabinoids can significantly increase the risk of psychosis and seizures. As a result, this combination should be strictly avoided.
- LSD
- Mescaline
- Mushrooms
- 25x-NBOMe
Legal status
 |
This legality section is a stub. As such, it may contain incomplete or wrong information. You can help by expanding it. |
- United States: Delta-8-THC is unregulated and is available without a prescription.
See also
External links
(List along order below)
- ↑ Adams, R., Cain, C. K., McPhee, W. D., & Wearn, R. B. (1941). Structure of cannabidiol. xii. isomerization to tetrahydrocannabinols1. Journal of the American Chemical Society, 63(8), 2209–2213. https://doi.org/10.1021/ja01853a052
- ↑ Hollister, L. E., & Gillespie, H. K. (1973). Delta-8- and delta-9-tetrahydrocannabinol; comparison in man by oral and Intravenous Administration. Clinical Pharmacology & Therapeutics, 14(3), 353–357. https://doi.org/10.1002/cpt1973143353
- ↑ 3.0 3.1 3.2 3.3 Robson, P. (2001). "Therapeutic aspects of cannabis and cannabinoids". The British Journal of Psychiatry. 178 (2): 107–115. doi:10.1192/bjp.178.2.107. ISSN 0007-1250.
- ↑ Mechoulam, Raphael; Parker, Linda A.; Gallily, Ruth (2002). "Cannabidiol: An Overview of Some Pharmacological Aspects". The Journal of Clinical Pharmacology. 42 (S1): 11S–19S. doi:10.1002/j.1552-4604.2002.tb05998.x. ISSN 0091-2700.
- ↑ Mechoulam, R. (1984). Cannabinoids as therapeutic agents. Boca Raton, FL: CRC Press. ISBN 0-8493-5772-1.
- ↑ Investigating the Neuroendocrine and Behavioral Controls of Cannabis-Induced Feeding Behavior. JF Davis, PQ Choi, J Kunze, P Wahl, Washington State University Pullman, WA, USA. Presented July 2018, Society for the Study of Ingestive Behavior, Bonita Springs, FL.
- ↑ Tetrahydrocannabivarin (THCV): A Cannabinoid Fighting Obesity | https://www.medicaljane.com/2013/08/27/tetrahydrocannabivarin-thcv-a-cannabinoid-fighting-obesity/
- ↑ Wong, MM; Craun, EA; Bravo, AJ; Pearson, MR; Protective Strategies Study, Team. (August 2019). "Insomnia symptoms, cannabis protective behavioral strategies, and hazardous cannabis use among U.S. college students". Experimental and clinical psychopharmacology. 27 (4): 309–317. doi:10.1037/pha0000273. PMID 30907602.
- ↑ The Pharmacologic and Clinical Effects of Medical Cannabis | http://onlinelibrary.wiley.com/doi/10.1002/phar.1187/abstract;jsessionid=1E004D7B7E2B5CA792E75A6E83EEC59C.f03t01
- ↑ The Therapeutic Potential of Cannabis and Cannabinoids | http://www.aerzteblatt.de/int/archive/article?id=127603
- ↑ Systematic Review and Meta-analysis of Cannabis Treatment for Chronic Pain | http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4637.2009.00703.x/abstract
- ↑ Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials | http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2125.2011.03970.x/abstract
- ↑ Yazulla, S (September 2008). "Endocannabinoids in the retina: from marijuana to neuroprotection". Progress in retinal and eye research. 27 (5): 501–26. doi:10.1016/j.preteyeres.2008.07.002. PMID 18725316.
- ↑ Charlotte Figi: The Girl Who is Changing Medical Marijuana Laws Across America | http://www.ibtimes.co.uk/charlotte-figi-girl-who-changing-medical-marijuana-laws-across-america-1453547
- ↑ On the frontier of medical pot to treat boy's epilepsy | http://articles.latimes.com/2012/sep/13/local/la-me-customized-marijuana-20120914
- ↑ Report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4157067/
- ↑ Cannabidiol displays antiepileptiform and antiseizure properties in vitro and in vivo. (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pubmed/19906779/
- ↑ An electrophysiological analysis of the anticonvulsant action of cannabidiol on limbic seizures in conscious rats. (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pubmed/477630
- ↑ Δ⁹-Tetrahydrocannabivarin suppresses in vitro epileptiform and in vivo seizure activity in adult rats. (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pubmed/20196794
- ↑ Cannabinoids: Defending the Epileptic Brain (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1176332/
- ↑ Is Marijuana an Effective Treatment for Glaucoma? | http://medicalmarijuana.procon.org/view.answers.php?questionID=000140
- ↑ Cardiovascular Effects of Cannabis | http://www.idmu.co.uk/canncardio.htm
- ↑ http://europepmc.org/abstract/med/1147519
- ↑ Lac, A; Luk, JW (February 2018). "Testing the Amotivational Syndrome: Marijuana Use Longitudinally Predicts Lower Self-Efficacy Even After Controlling for Demographics, Personality, and Alcohol and Cigarette Use". Prevention science : the official journal of the Society for Prevention Research. 19 (2): 117–126. doi:10.1007/s11121-017-0811-3. PMID 28620722.
- ↑ Feinberg, I., Jones, R, Walker JM, Cavness, C, March, J. (1975). Effects of high dosage delta-9-tetrahydrocannabinol on sleep patterns in man. Clin Parmacol Ther. 1975; 17(4):458-66.
- ↑ https://psychonautwiki.org/wiki/Laughter_fits
- ↑ Causal association between cannabis and psychosis: examination of the evidence - The British Journal of Psychiatry Jan 2004, 184 (2) 110-117 | http://bjp.rcpsych.org/content/184/2/110.short
- ↑ A Teenager With Agitation: Higher Than She Should Have Climbed - Pediatric Emergency Care: June 2010 - Volume 26 - Issue 6 - pp 462-465 | http://journals.lww.com/pec-online/Abstract/2010/06000/A_Teenager_With_Agitation__Higher_Than_She_Should.16.aspx
- ↑ Development of a rational scale to assess the harm of drugs of potential misuse (ScienceDirect) | http://www.sciencedirect.com/science/article/pii/S0140673607604644
- ↑ Sorensen, Cecilia J.; DeSanto, Kristen; Borgelt, Laura; Phillips, Kristina T.; Monte, Andrew A. (20 December 2016). "Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment—a Systematic Review". Journal of Medical Toxicology. 13 (1): 71–87. doi:10.1007/s13181-016-0595-z. PMC 5330965
 . PMID 28000146.
. PMID 28000146.
- ↑ DeVuono, Marieka; Parker, Linda (2020). "Cannabinoid Hyperemesis Syndrome: A Review of Potential Mechanisms". Cannabis and Cannabinoid Research. 5: 132–144. doi:10.1089/can.2019.0059.
- ↑ El Omri, N; Eljaoudi, R; Mekouar, F; Jira, M; Sekkach, Y; Amezyane, T; Ghafir, D (2017). "Cannabis arteritis". The Pan African medical journal. 26: 53. doi:10.11604/pamj.2017.26.53.11694. PMID 28451030.
- ↑ https://www.nih.gov/news-events/news-releases/canSuicidality
- ↑ https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/cannabis-and-suicide-longitudinal-study/6CFEC0A5B314F34D35A68693A847CAAD
- ↑ https://www.sciencedirect.com/science/article/abs/pii/S0165032715310004
- ↑ Causal association between cannabis and psychosis: examination of the evidence - The British Journal of Psychiatry Jan 2004, 184 (2) 110-117 | http://bjp.rcpsych.org/content/184/2/110.short
- ↑ Every-Palmer, S. Synthetic cannabinoid use and psychosis: an explorative study. Journal of Drug and Alcohol Dependence 2011.
- ↑ “Spice” Girls: Synthetic Cannabinoid Intoxication - The Journal of Emergency Medicine Volume 40, Issue 3, March 2011, Pages 296–299 (ScienceDirect) | http://www.sciencedirect.com/science/article/pii/S0736467910008802
- ↑ A Teenager With Agitation: Higher Than She Should Have Climbed - Pediatric Emergency Care: June 2010 - Volume 26 - Issue 6 - pp 462-465 | http://journals.lww.com/pec-online/Abstract/2010/06000/A_Teenager_With_Agitation__Higher_Than_She_Should.16.aspx
- ↑ Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use | http://onlinelibrary.wiley.com/doi/10.1111/j.1465-3362.2009.00149.x/abstract
- ↑ Pharmacology and effects of cannabis: a brief review | http://bjp.rcpsych.org/content/178/2/101
- ↑ Adverse effects of cannabis | http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(98)05021-1/fulltext
- ↑ https://www.drugbank.ca/drugs/DB00470
- ↑ Tetrahydrocannabinols in clinical and forensic toxicology (PubMed.gov / NCBI) | http://www.ncbi.nlm.nih.gov/pubmed/16225128
- ↑ Cannabinoid Hyperemesis Syndrome | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3576702/
- ↑ Cannabinoid Hyperemesis Syndrome: Reports of Fatal Cases | https://pubmed.ncbi.nlm.nih.gov/29768651/
- ↑ Lopez-Quintero C, Pérez de los Cobos J, Hasin DS, et al.: Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend 2011; 115: 120–30 | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3069146/
- ↑ The Pharmacologic and Clinical Effects of Medical Cannabis | http://onlinelibrary.wiley.com/doi/10.1002/phar.1187/abstract
- ↑ The Effect of Cannabis Compared with Alcohol on Driving | http://onlinelibrary.wiley.com/doi/10.1080/10550490902786934/abstract
- ↑ Medical Consequences of Marijuana Use: A Review of Current Literature | http://link.springer.com/article/10.1007%2Fs11920-013-0419-7
- ↑ State of the Art Treatments for Cannabis Dependence (ScienceDirect) | http://www.sciencedirect.com/science/article/pii/S0193953X12000202
- ↑ Cannabinoid tolerance and dependence | http://www.ncbi.nlm.nih.gov/pubmed/16596793
- ↑ MARIJUANA AND MEDICINE Assessing the Science Base | http://www.nap.edu/openbook.php?record_id=6376
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/3902318
- ↑ Winstock AR, Ford C, Witton J. Assessment and management of cannabis use disorders in primary care. BMJ. 2010;340:c1571. PubMed doi:10.1136/bmj.c1571