Substance withdrawal
Substance withdrawal is a group of symptoms that occur upon the abrupt discontinuation or decrease in one's intake of a substance. Withdrawal develops after a physical or mental dependence, which is caused by consuming substances for an extended period of time. It is dose dependent and varies based upon the substance consumed, the duration of intake, as well as the route of administration used.
Each substance causes its own specific symptoms with opioid withdrawals causing significantly different symptoms than benzodiazepine withdrawal, for instance. The term "cold turkey" is used to describe the sudden cessation use of a substance and the ensuing physiologic manifestations. It is recommended that users taper their dose slowly over time instead of abruptly stopping, which is associated with higher rates of relapse.[avoid opinion][citation needed]
Death can occur from the withdrawal of GABAergic substances such as benzodiazepines, thienodiazepines, alcohol, or barbiturates, so tapering is especially recommended for these substances, ideally under medical supervision.[1][2][3]
Opioid withdrawal
Withdrawal symptoms are commonly reported following abuse of opioids (such as heroin, hydrocodone, or oxycodone) over an extended period of time. They are also present with the newer brand of research chemicals such as U-47700 and fentanyl analogs. Withdrawal is not expected to occur in opioid-naive individuals or those who use infrequently, as it is caused by the down-regulation of opioid receptors in response to repeated usage. The experience of opioid withdrawal is often described as being "flu-like" in nature and includes rebound sensitivity to pain and tactile stimulation.
Opioids with a short half-life, such as diacetylmorphine (heroin) are well known to induce withdrawal symptoms in tolerant individuals within several hours of having cleared the body. Longer eliminating opioids like methadone will exhibit symptoms of withdrawal much later, but the effects will linger far in excess of shorter acting opioids. Faster eliminating opioids like Fentanyl and U47700 will exhibit the symptoms of withdrawal much quicker, but the effects will subside faster than longer acting opioids such as heroin.
Withdrawal symptoms from opiate abuse include (but are not limited to):
- Anxiety
- Insomnia
- Cravings
- Altered perception of temperature (hot/cold flashes)
- Abdominal cramping
- Nausea and vomiting
- Motivation suppression
- Appetite suppression
- Depression - This effect should be monitored closely as it can lead to suicidal idealizations[4]
- Diarrhea
- Dehydration
- Muscle fatigue
- Muscle aches - In addition to muscle pain and aches, joint and bone pain are also present.
- Restless legs syndrome
- Runny nose
- Sneezing
- Excessive yawning
- Skin crawling - This is distinct from the goosebumps experienced in withdrawal because the skin crawling sensation feels like something is distinctly moving under the skin.
- Goosebumps - These are raised areas on the skin[5] that can appear and disappear suddenly.
- Sweating
- Dilated pupils - These are a stark contrast to the constricted pupils one sees in active opiate abusers and can be a hallmark of late stage opiate withdrawal.[4]
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining substance should be given to a trusted friend or family member and distributed by only them.
- Opioid replacement therapy (ORT) - Methadone and buprenorphine (Suboxone) are longer acting but less recreational opioids that are often used to relieve opioid cravings, suppress withdrawal symptoms, and block the euphoric effects associated with opioids. However, methadone has severe withdrawal symptoms lasting multiple weeks, so this should be considered when choosing a method of treatment. When using replacement substances, it is highly recommended to gradually lower one's intake at the recommendation of a physician instead of abruptly stopping.
- Over-the-counter painkillers - OTC painkillers such as naproxen, aspirin, acetaminophen, or ibuprofen can reduce withdrawal symptoms and lessen pain.
- Weak opioids (kratom, codeine, or tianeptine) - Switching to a weaker opioid can lessen the perceived symptoms, but is likely to also prolong the period of withdrawal and could potentially lead to addiction.
- Gabapentin or pregabalin - Both of these prescription medicines can prevent or lessen restless legs syndrome.
- Clonidine - Clonidine is a prescription alpha-2 adrenal agonist that is often prescribed to help alleviate some of the symptoms of opioid withdrawal.
- Loperamide - Loperamide (Immodium) is an over-the-counter medicine used to treat diarrhea. It acts on the opioid receptors in the intestines and has no appreciable effect on the central nervous system. Therapeutic doses may help relieve some gastrointestinal issues stemming from opioid withdrawal.
- Dextromethorphan (DXM) - DXM may help with opioid withdrawal. The reasons for this are not entirely clear, but many people have reported a mild or moderate benefit from using DXM as a withdrawal remedy.
- Diphenhydramine (DPH) - Some users report that DPH can mildly reduce withdrawals and assist with sleep.
- Benzodiazepines - As benzodiazepines have a high risk of addiction, one should be careful not to become physically dependent on them. They can aid in sleep and muscle cramps for withdrawal but should be used sparingly.
Alcohol withdrawal
The withdrawal symptoms of alcohol occur six hours after the abrupt discontinuation of extended alcohol usage. They are at their worst between 24 and 72 hours and improvement typically occurs by the seventh day.[6] The mechanism which underlies this process involves a decrease responsiveness of GABA receptors in the brain.
Due to the risk of seizures or delirium tremens, alcohol withdrawal can be fatal depending on the severity of usage. It is recommended to taper one's dosage and to seek medical attention and begin treatment as soon as possible.
Alcohol abuse withdrawal symptoms include:
- Anxiety[6]
- Fever
- Tremors[6]
- Seizures[6] - In severe cases, this can result in death. Seizures typically occur within 48 hours of the abrupt discontinuation of alcohol and occur either as a single generalized tonic-clonic seizure or as a brief episode of multiple seizures.[7]
- External hallucinations[6]
- Auditory hallucinations[6]
- Tactile hallucinations[6]
- Increased heart rate[6]
- Irritability
- Delirium tremens - This is the rapid onset of delirium, confusion, hallucinations, and other symptoms associated with alcohol withdrawal caused by the abrupt discontinuation in long-term/heavy users. Delirium tremens are a cluster of symptoms, which can be potentially fatal. Delirium tremens usually occur three days after discontinuation and can last up to three days. It is reported that they are characteristically worse at night. Anyone thought to be suffering from the condition requires immediate medical intervention due to the risk of death, with the mortality without treatment being between 15% and 40%.[8]
- Increased blood pressure[6]
- Dream potentiation - For many individuals this can often lead to particularly unsettling, scary and abnormally vivid dreams or nightmares.
- Cognitive fatigue
- Physical fatigue
- Headaches[6]
- Shaking
- Increased perspiration
- Nausea[6]
- Wernicke syndrome - This is condition characterized by extreme confusion, an abnormal gait, and the paralysis of muscles in the eye. This condition occurs only in severe alcohol withdrawal cases. Wernicke syndrome can progress into irreversible dementia so anyone suspected of this should seek immediate medical attention and be treated with 100mg of thiamine daily while withdrawling.[9]
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining alcohol should be given to a trusted friend or family member and distributed by only them.
- Benzodiazepines - Benzodiazepines (such as diazepam, lorazepam, chlordiazepoxide, and oxazepam) are the most common treatment for alcohol withdrawal.[10] However, benzodiazepines have a high risk of addiction, so one should be careful not to become physically dependent on them.
- Vitamins such as thiamine[11], folic acid, and pyridoxine - These vitamins are often recommended because those dependent on alcohol are often deficient in nutrients; in very severe cases, this can result in Wernicke syndrome, which is a condition characterized by extreme confusion, an abnormal gait, and the paralysis of muscles in the eye. Wernicke syndrome can progress into irreversible dementia so anyone suspected of this should seek immediate medical attention and be treated with 100mg of thiamine daily while withdrawling.
- Magnesium - Although it has not been verified, there may be a causal relationship between low magnesium levels and withdrawal seizures or delirium.[9]
- Anticonvulsants such as topiramate, pregabalin, or gabapentin - There is some limited evidence that topiramate, pregabalin, or gabapentin could help alcohol withdrawal; however, gabapentin is not recommended for severe withdrawal.[12][13]
- Haloperidol - The antipsychotic haloperidol may also be used to control symptoms, especially agitation or psychosis. However, antipsychotics lower the seizure threshold so they can potentially worsen the withdrawal.
- Paraldehyde - This is an older medication that is generally not used anymore. In regards to treating severe and fatal withdrawal symptoms, paraldehyde combined with chloral hydrate showed superior results over chlordiazepoxide.[14]
- Acamprosate - This substance is sometimes used in addition to other treatments. It can be continued long-term to reduce the risk of relapse.
- Carbamazepine - This substance assisted in the reduction of withdrawal symptoms in seven scientific trials involving 612 patients.[9]</ref> However, it is questionable whether or not the substance can prevent seizures and delirium tremens in a similar manner to benzodiazepines due to inconclusive evidence.
- Clonidine - This substance is sometimes combined with benzodiazepines to treat symptoms.
Nicotine withdrawal
While nicotine withdrawal may cause some withdrawal effects, it is not life-threatening. However, the mental cravings which it can induce can be as intense as other addictive substances such as alcohol.
The effects generally begin 2-3 hours after cessation, peak in 2-3 days, and last 2-4 weeks.
Withdrawal from nicotine includes:
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's intake of nicotine over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. This may be very difficult for some individuals and many prefer to quit cold turkey.
- Nicotine replacement therapy - This stops withdrawal symptoms by providing the body with an alternative source of nicotine. NRT is available in numerous forms and includes nicotine chewing gum, adhesive patches, lozenges, and nasal sprays.[15] Combining different forms is shown to be more effective than only using one form.[16][17] Generally, the user is encouraged to later taper one's new nicotine intake after several weeks.
- Bupropion (Wellbutrin) - This is a medication primarily used as an antidepressant and smoking cessation aid, reducing the intensity of nicotine cravings and its withdrawal symptoms. It acts as a nicotinic acetylcholine receptor antagonist as well as a noradrenaline-dopamine reuptake inhibitor (NDRI). It doubles the chance of quitting smoking successfully, making its effectiveness comparable to nicotine replacement therapy but less effective than varenicline.[18]
- Varenicline (Chantix) - This prescription medication is a nicotinic receptor partial agonist which is similar to cytisine and works to reduce cravings by stimulating nicotine receptors more weakly than nicotine itself does. It also decreases the euphoric effects of cigarettes and other nicotine products.
- Cytisine - This substance is a partial agonist of nicotinic acetylcholine receptors (nAChRs), which is similar to varenicline.
- Exercise - Non-medications treatments such as increased exercise can also reduce nicotine withdrawal.
- NAC - In terms of reducing cravings, NAC has been shown to provide relief for those who struggle with compulsive redosing and psychological cravings.
Other medications used for quitting smoking include nortriptyline and clonidine. Many behavior changes such as avoiding situations where one usually smoked, planning ahead to deal with temptations, and seeking the support of friends and family are effective in helping people quit smoking, but whether this is due to reduced withdrawal is unclear.
Benzodiazepine withdrawal
Due to the risk of seizures, benzodiazepine withdrawal can be fatal depending on the severity of usage. It is recommended to taper one's dosage, and seek medical attention to begin treatment as soon as possible if one has been using for a long time or is experiencing severe symptoms. Short-acting benzodiazepines usually present withdrawal symptoms after 24 to 48 hours; however, it can take a couple weeks for the symptoms of longer lasting ones to appear.
A small minority of users who abuse benzodiazepines for extended periods of time may develop post-acute-withdrawal syndrome, which may last for months or years after stopping usage.
The following symptoms may emerge during gradual or abrupt dosage reduction:
- Aches and pains
- Anxiety and panic attacks
- Visual acuity suppression (Blurred vision)
- Chest pain
- Depersonalization
- Depression
- Derealisation (feelings of unreality)
- Diarrhea
- Dizziness
- Double vision
- Dry mouth
- Cognitive dysphoria
- Brain zaps
- Increased blood pressure
- Cognitive fatigue
- Physical fatigue
- Ear ringing
- Headaches
- Hot and cold spells
- Hypertension
- Tactile enhancement
- Increased sensitivity to sound
- Increased urinary frequency
- Insomnia
- Focus suppression
- Memory suppression
- Appetite suppression
- Gustatory hallucinations - This may present as a metallic taste.
- Mild to moderate aphasia
- Mood swings
- Muscle spasms, cramps or fasciculations
- Nausea and vomiting
- Dream potentiation
- Numbness and tingling
- Paranoia
- Increased perspiration
- Photophobia
- Restless legs syndrome
- Tachycardia
- Tinnitus
- Catatonia - This may result in death.[19]
- Confusion
- Seizures - This may result in death.[20]
- Coma (rare)
- Delirium tremens
- Delusions
- Hallucinations
- Increased bodily temperature
- Mania
- Psychosis
- Suicidal ideation
Treatment
- Tapering - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining substance should be given to a trusted friend or family member and distributed by only them.
- Gabapentin or pregabalin
- Baclofen[21]
- Phenibut - Switching to another GABAergic can lessen the perceived symptoms, but is likely to also prolong the period of withdrawal and could potentially lead to addiction.
- L-Theanine
- Melatonin - This may help with sleep.
- Valerian root
- GABA - Although GABA may not cross the blood-brain barrier, there are some reports of this supplement helping withdrawal.
- Magnesium[22]
- Flumazenil
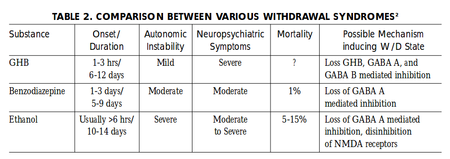
GHB, GBL, and 1,4-butanediol withdrawal
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining substance should be given to a trusted friend or family member and distributed by only them.
Cannabis withdrawal
Although not medically serious, cannabis withdrawal symptoms can occur in users who have been using the substance for an extended period of time. In comparison to most other substances, cannabis withdrawal is very mild. Most symptoms begin during the first week of abstinence and resolve after a few weeks. These symptoms include:
- Anger
- Cognitive dysphoria
- Anxiety
- Irritability
- Depression
- Dream potentiation
- Ear ringing (rare)
- Restlessness
- Insomnia
- Gastrointestinal symptoms
- Appetite suppression
- Nausea
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining substance should be given to a trusted friend or family member and distributed by only them.
- Dronabinol - Dronabinol is an agonist that is legally available; in some cases and trials, it reduced symptoms of withdrawal and reduced cannabis use.[24]
- Diphenhydramine (DPH) - This substance can assist with sleep if one has insomnia, but may also exacerbate the restlessness of withdrawal in high does.
- Benzodiazepines - As benzodiazepines have a high risk of addiction, one should be careful not to become physically dependent on them.
- Exercise - This may reduce some symptoms and accelerates the rate that THC exits the body by releasing the THC metabolites stored in the fat tissue into the blood stream[25].
- N-Acetylcysteine (NAC) - In terms of reducing cravings, NAC has been shown to provide relief for those who struggle with compulsive redosing and psychological cravings with cocaine, and has been singled out with gabapentin as a promising potential treatment for cannabis-dependent users.[26][27]
- Magnesium - Magnesium supplementation can be used to help treat some of the anxiety of cannabis withdrawal as well as the potential mental and physical restlessness that often accompanies it.[citation needed]
- Gabapentin - Early, preliminary evidence suggests that gabapentin is capable of reducing withdrawal symptoms and relapse rates in cannabis-dependent adults who seek to quit. However, larger confirmatory studies are still required.[28]
- Acetaminophen (paracetamol) - Acetaminophen (paracetamol) may help with withdrawal due to one of its metabolites being a cannabinoid (CB1) agonist.[citation needed]
Caffeine withdrawal
Research has suggested that withdrawals start between 12 to 24 hours after the abrupt discontinuation of caffeine and may last up to nine days.[29]
Caffeine dependence can involve withdrawal symptoms such as:
- Headaches - In one study, it was found that headaches were experienced by half of the participants who stopped consuming 235mg of caffeine on average daily for two days.[30]
- Physical fatigue[31]
- Decreased energy[31]
- Depression[31]
- Focus suppression[31]
- Sleepiness[31]
- Stomach pain
- Muscle pain[31]
- Joint pain
- Irritability[31]
- Nausea and vomitting[31]
- Anxiety[31]
- Cravings[31]
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. The amount of caffeine present in a drink is usually written on the nutrition facts or is searchable online. For an easy taper, buy caffeine pills and then divide the doses into halves and eventually quarters using a pill cutter. If you are unable to control yourself from dosing too high, the remaining substance should be given to a trusted friend or family member and distributed by only them.
- Over-the-counter painkillers - Painkillers such as naproxen, aspirin, acetaminophen, or ibuprofen can reduce withdrawal symptoms such as headaches and lessen any muscle or joint pain. Some OTC products include caffeine alongside painkillers, which can be used to self-administer a taper.
Stimulant withdrawal
Stimulants include amphetamine, cocaine, and methamphetamine.
Symptoms of stimulant withdrawal include:
- Paranoia[32]
- Cravings[32]
- Physical fatigue[32]
- Insomnia[32]
- Depression[32]
- Anxiety[32]
- Irritability[32]
Treatment
- Gradually tapering one's intake - Withdrawal symptoms can be reduced by slowly lowering one's dosage over a period of days or weeks, which will let receptors recover somewhat before complete discontinuation. This will lessen the severity of symptoms but likely prolong their duration. It is inadvisable to self-administer a taper; the remaining substance should be given to a trusted friend or family member and distributed by only them.
- NAC - In terms of reducing cravings, NAC has been shown to provide relief for those who struggle with compulsive redosing and psychological cravings.
See also
References
- ↑ Lann, M. A., Molina, D. K. (June 2009). "A fatal case of benzodiazepine withdrawal". The American Journal of Forensic Medicine and Pathology. 30 (2): 177–179. doi:10.1097/PAF.0b013e3181875aa0. ISSN 1533-404X.
- ↑ Mirijello, A., D’Angelo, C., Ferrulli, A., Vassallo, G., Antonelli, M., Caputo, F., Leggio, L., Gasbarrini, A., Addolorato, G. (March 2015). "IDENTIFICATION AND MANAGEMENT OF ALCOHOL WITHDRAWAL SYNDROME". Drugs. 75 (4): 353–365. doi:10.1007/s40265-015-0358-1. ISSN 0012-6667.
- ↑ Sarrecchia, C., Sordillo, P., Conte, G., Rocchi, G. (December 1998). "[Barbiturate withdrawal syndrome: a case associated with the abuse of a headache medication]". Annali Italiani Di Medicina Interna: Organo Ufficiale Della Societa Italiana Di Medicina Interna. 13 (4): 237–239. ISSN 0393-9340.
- ↑ 4.0 4.1 Opiate and opioid withdrawal: MedlinePlus Medical Encyclopedia
- ↑ goosebumps
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Simpson, S. A., Wilson, M. P., Nordstrom, K. (September 2016). "Psychiatric Emergencies for Clinicians: Emergency Department Management of Alcohol Withdrawal". The Journal of Emergency Medicine. 51 (3): 269–273. doi:10.1016/j.jemermed.2016.03.027. ISSN 0736-4679.
- ↑ Manasco, A., Chang, S., Larriviere, J., Hamm, L. L., Glass, M. (November 2012). "Alcohol withdrawal". Southern Medical Journal. 105 (11): 607–612. doi:10.1097/SMJ.0b013e31826efb2d. ISSN 1541-8243.
- ↑ Blom, J. D. (8 December 2009). A Dictionary of Hallucinations. Springer Science & Business Media. ISBN 9781441912237.
- ↑ 9.0 9.1 9.2 Myrick, H., Anton, R. F. (1998). "Treatment of Alcohol Withdrawal". Alcohol Health and Research World. 22 (1): 38–43. ISSN 0090-838X.
- ↑ Stern, T. A., Gross, A. F., Stern, T. W., Nejad, S. H., Maldonado, J. R. (2010). "Current approaches to the recognition and treatment of alcohol withdrawal and delirium tremens: "old wine in new bottles" or "new wine in old bottles"". Primary Care Companion to the Journal of Clinical Psychiatry. 12 (3): PCC.10r00991. doi:10.4088/PCC.10r00991ecr. ISSN 1555-211X.
- ↑ Schuckit, M. A. (27 November 2014). "Recognition and management of withdrawal delirium (delirium tremens)". The New England Journal of Medicine. 371 (22): 2109–2113. doi:10.1056/NEJMra1407298. ISSN 1533-4406.
- ↑ Hammond, C. J., Niciu, M. J., Drew, S., Arias, A. J. (April 2015). "Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders". CNS drugs. 29 (4): 293–311. doi:10.1007/s40263-015-0240-4. ISSN 1179-1934.
- ↑ Leung, J. G., Hall-Flavin, D., Nelson, S., Schmidt, K. A., Schak, K. M. (August 2015). "The role of gabapentin in the management of alcohol withdrawal and dependence". The Annals of Pharmacotherapy. 49 (8): 897–906. doi:10.1177/1060028015585849. ISSN 1542-6270.
- ↑ Minozzi, S., Amato, L., Vecchi, S., Davoli, M. (17 March 2010). Cochrane Drugs and Alcohol Group, ed. "Anticonvulsants for alcohol withdrawal". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD005064.pub3. ISSN 1465-1858.
- ↑ Nicotine (Drugs.com) | https://www.drugs.com/monograph/nicotine.html
- ↑ McDonough, M. (August 2015). "Update on medicines for smoking cessation". Australian Prescriber. 38 (4): 106–111. doi:10.18773/austprescr.2015.038. ISSN 0312-8008.
- ↑ Cahill, K., Stevens, S., Perera, R., Lancaster, T. (31 May 2013). "Pharmacological interventions for smoking cessation: an overview and network meta-analysis". The Cochrane Database of Systematic Reviews (5): CD009329. doi:10.1002/14651858.CD009329.pub2. ISSN 1469-493X.
- ↑ Wu, P., Wilson, K., Dimoulas, P., Mills, E. J. (11 December 2006). "Effectiveness of smoking cessation therapies: a systematic review and meta-analysis". BMC public health. 6: 300. doi:10.1186/1471-2458-6-300. ISSN 1471-2458.
- ↑ Rosebush, P. I., Mazurek, M. F. (August 1996). "Catatonia after benzodiazepine withdrawal". Journal of Clinical Psychopharmacology. 16 (4): 315–319. doi:10.1097/00004714-199608000-00007. ISSN 0271-0749.
- ↑ Haque, W., Watson, D. J., Bryant, S. G. (January 1990). "Death following suspected alprazolam withdrawal seizures: a case report". Texas Medicine. 86 (1): 44–47. ISSN 0040-4470.
- ↑ Shukla, L., Kandasamy, A., Kesavan, M., Benegal, V. (November 2014). "Baclofen in the short-term maintenance treatment of benzodiazepine dependence". Journal of Neurosciences in Rural Practice. 5 (Suppl 1): S53–S54. doi:10.4103/0976-3147.145203. ISSN 0976-3147.
- ↑ Hantouche, E. G., Guelfi, J. D., Comet, D. (October 1998). "[alpha-beta L-aspartate magnesium in treatment of chronic benzodiazepine abuse: controlled and double-blind study versus placebo]". L’Encephale. 24 (5): 469–479. ISSN 0013-7006.
- ↑ GHB Withdrawal Syndrome | Texas Commission on Alcohol and Drug Abuse | https://www.erowid.org/chemicals/ghb/ghb_addiction2.pdf
- ↑ Danovitch, I., Gorelick, D. A. (June 2012). "State of the Art Treatments for Cannabis Dependence". The Psychiatric Clinics of North America. 35 (2): 309–326. doi:10.1016/j.psc.2012.03.003. ISSN 0193-953X.
- ↑ Gunasekaran, N., Long, L., Dawson, B., Hansen, G., Richardson, D., Li, K., Arnold, J., McGregor, I. (November 2009). "Reintoxication: the release of fat-stored Δ9-tetrahydrocannabinol (THC) into blood is enhanced by food deprivation or ACTH exposure". British Journal of Pharmacology. 158 (5): 1330–1337. doi:10.1111/j.1476-5381.2009.00399.x. ISSN 0007-1188.
- ↑ Nocito Echevarria, M. A., Andrade Reis, T., Ruffo Capatti, G., Siciliano Soares, V., Silveira, D. X. da, Fidalgo, T. M. (May 2017). "N-acetylcysteine for treating cocaine addiction – A systematic review". Psychiatry Research. 251: 197–203. doi:10.1016/j.psychres.2017.02.024. ISSN 0165-1781.
- ↑ Sherman, B. J., McRae-Clark, A. L. (May 2016). "Treatment of Cannabis Use Disorder: Current Science and Future Outlook". Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 36 (5): 511–535. doi:10.1002/phar.1747. ISSN 0277-0008.
- ↑ Mason, B. J., Crean, R., Goodell, V., Light, J. M., Quello, S., Shadan, F., Buffkins, K., Kyle, M., Adusumalli, M., Begovic, A., Rao, S. (June 2012). "A Proof-of-Concept Randomized Controlled Study of Gabapentin: Effects on Cannabis Use, Withdrawal and Executive Function Deficits in Cannabis-Dependent Adults". Neuropsychopharmacology. 37 (7): 1689–1698. doi:10.1038/npp.2012.14. ISSN 0893-133X.
- ↑ Juliano, L. M., Griffiths, R. R. (October 2004). "A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features". Psychopharmacology. 176 (1): 1–29. doi:10.1007/s00213-004-2000-x. ISSN 0033-3158.
- ↑ Silverman, K., Evans, S. M., Strain, E. C., Griffiths, R. R. (15 October 1992). "Withdrawal syndrome after the double-blind cessation of caffeine consumption". The New England Journal of Medicine. 327 (16): 1109–1114. doi:10.1056/NEJM199210153271601. ISSN 0028-4793.
- ↑ 31.0 31.1 31.2 31.3 31.4 31.5 31.6 31.7 31.8 31.9 JJuliano, L. M., Griffiths, R. R. (October 2004). "A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features". Psychopharmacology. 176 (1): 1–29. doi:10.1007/s00213-004-2000-x. ISSN 0033-3158.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 Treatment for Stimulant Use Disorders - U.S. Department of Health and Human Services (Samhsa.gov) | https://store.samhsa.gov/shin/content/QGCT33/QGCT33.pdf