Safer injection guide

Using and sharing injection materials (including spoons) can cause serious injury and death.
Using and sharing injection equipment is an extremely high-risk activity and is never truly safe to do in a nonmedical context. This guide is provided for educational and harm reduction purposes, and we strongly discourage irresponsible users from engaging in this activity.
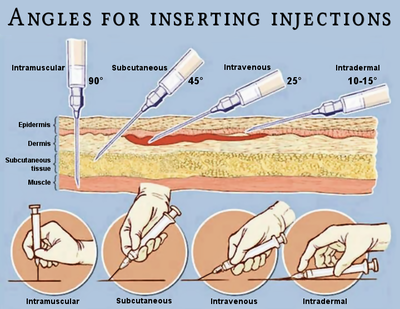
Injection is the act of delivering a psychoactive substance into the body using a hypodermic needle. Injected substances are mixed with a liquid (such as sterilie water for injection) to form a solution, which is usually either injected directly into the bloodstream via the veins (i.e. intravenous or IV injection) or into the muscle tissue (i.e. intramuscular or IM injection).
Injecting substances removes any bodily filtering mechanism and IV injection results in 100% bioavailability of a substance.[5] Any impurities present in the product will pose a significantly greater health threat. Even medical grade substances specifically manufactured for injection carry a risk of infection and death. As a result, this guide has been deliberately named the "safe(r) injection guide" to emphasize the fact that there is no such thing as truly safe injection.
While most psychoactive substances are capable of being injected, the practice is most commonly associated with opiates like heroin, stimulants like methamphetamine and cocaine, and dissociatives.
When using opiates it is highly recommended to have naloxone nasal spray, available for free at some pharmacies, in order to reverse the effects of the opiate, and then call or get someone to call emergency services, as multiple doses of the naloxone are needed in order to continue effects, which first responders and the hospital will have. This can save a life.
Risks and hazards
See also Dangers specific to IV drug use.
Health problems arise from poor hygiene and injection technique (be it IV, IM, or SC), such as cotton fever, phlebitis, abscesses, vein collapse, ulcers, malaria, gas gangrene, tetanus, septicaemia, thrombosis, embolism and all results thereof. Drug injection is also commonly a component in HIV-related syndemics.
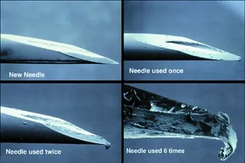
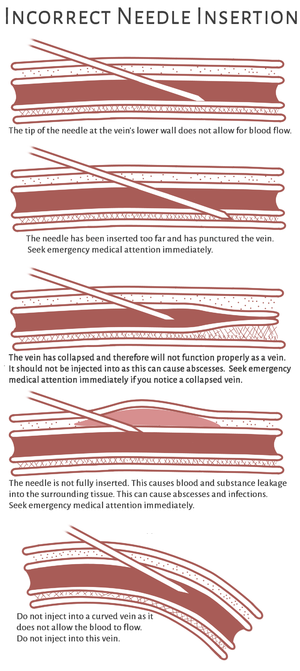
- Reusing hypodermic needles - Reusing needles (including stainless steel hypodermic needles that can be autoclaved) is not advised for a number of medical reasons. If upon injection the needle does not hit a vein or muscle tissue, only retry with that same needle one more time if needed. It is always best to use fresh needles for each injection because needles are designed to penetrate the surface of the skin only once. After the first use, the needle becomes dulled and each additional time increases the dullness. Reusing the same needle can lead to greater risk of bodily injury and abscessed infections. Fresh needles can be found at needle exchange programs in certain areas. Needles that have been re-used many times will get macro trauma to the needle tip, resulting in a hook shape. If the needle gets hooked when injected it will cause tissue damage (e.g. a collapsed vein when taken intravenously) when it is pulled out.
- Increased risk of infection - The simple act of penetrating the skin with anything is a way to introduce bacteria and viruses directly into the body. One should be as sterile as humanly possible when injecting, making sure to use alcohol swabs to wipe the injection area before and after injection. There is also the risk of infection if the injected substance is impure, adulterated, or unfiltered, which is extremely common. These substances do not pass any membrane for filtration, and any impurity in the substance will therefore be directly introduced into the body.[6] People who inject are at an increased risk of bacterial infections such as MRSA.[7]
- Blood-borne diseases - Sharing spoons (or other containers), syringes, and/or hypodermic needles with other users is the most obvious way to transmit a blood-borne disease or infection, but there are other ways too. Using multiple needles in the same water supply can easily spread illness and disease. Sharing the same spoons and other equipment used to prepare the injection solution is also a way to contract a blood-borne illness such as HIV/AIDS or Hepatitis B & C.[7] Refer to the sharing injection materials page for more information about the sharing of injection materials and the inherent risks of contracting infection and disease.
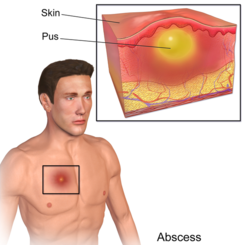
- Abscessed infections - An abscessed infection is a collection of pus (usually caused by a bacterial infection) that has built up within the tissue of the body at or underneath an administration site.[8] If one notices an abscess forming following an injection, they should seek professional medical help immediately because abscessed infections can lead to severe health complications and, not uncommonly, death. Abscessed infections are especially common when IV injecting into the feet, as the blood circulation in the extremities is poor and decreases the foot's ability to heal.
- Endocarditis - an inflammation of the inner layer of the heart, the endocardium.
- Gangrene - If one injects into an artery or muscle tissue, a gangrenous infection may develop.[9]
- Increased withdrawal effects - This is observed with many substances such as opiates, methamphetamine, and cocaine. The higher bioavailability and shorter time to reaches peak blood plasma levels (i.e. "rushiness") of the substance when it is injected along with increased cognitive euphoria and physical euphoria that accompanies it is thought to contribute substantially to compulsive use, addiction, withdrawal, and persisting substance cravings long after cessation of use.
- Intensified comedowns - Substances that have comedowns, such as stimulants and U-47700, have a greatly exacerbated comedown when injected. This means that the symptoms of a comedown, such as depression, anxiety, cognitive fatigue, and motivation suppression are intensified and harder to deal with, which could lead to compulsive redosing.
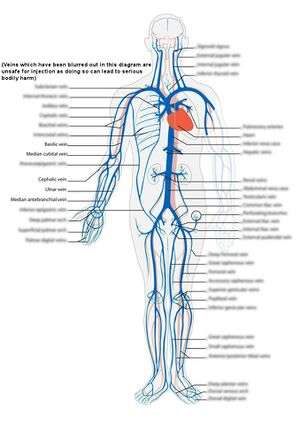
- Stroke risk - Injecting into an artery and not a vein can be a potential cause of strokes and blood embolisms. This risk is especially present with IV drug use, when one misses a vein and injects into the artery instead. This is why it is important to make sure one is in a vein before IV injection. This risk increases with the use of uncommon injection sites such as the neck: the chemicals being injected might enter an artery and go straight to the brain, causing neurological problems and strokes.[10]
- Nerve damage - Injecting into the muscle tissue during an IM injection, missing a vein during IV injection, and SC injecting can all present the risk of nerve damage. The hypodermic needle may puncture a nerve and cause serious, painful, and possibly fatal bodily harm. This risk is especially present if injecting into the groin, as the femoral nerve located there controls leg and muscle movement - damaging this nerve can result in serious problems with mobility or even paralysis.[10]
- Deep Vein Thrombosis (DVT) - Deep vein thrombosis is a blood clot occurring in the deep arms of the legs and extremities, especially the legs.[11] This is a risk that is especially present with IV drug use into the groin are and the deep veins in the arm. Signs of deep vein thrombosis include; pain, swelling, redness, or tenderness of the leg or arm around the injection site. IV drug use leads to a higher rate of DVT in younger patients, with most DVT issues occurring in the groin area and the thigh.[12]
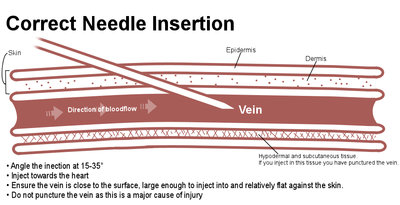
- Hitting an artery - One should always inject into a vein and never inject into an artery. One can differ between a vein and an artery by the following signs: Upon injection, when the plunger is pulled down the pressure of the blood in the artery will push it back up. The blood in the syringe is bright red, frothing and gushing versus the dark red and slow moving blood found within veins. You can avoid hitting an artery by never injecting where you feel a pulse and never trying to IV inject into deeper veins than those at the surface.
- Development of scar tissue - This is especially present with IV injection, but can occur with IM and SC injections as well. If the site of injection is not varied, scar tissue can develop and can impede further injections.
- Extravasation - Extravasation is the leakage of intravenously (IV) infused, and potentially damaging, medications into the extravascular tissue around the site of infusion. Extravasation of medication during intravenous therapy is an adverse event related to therapy that can potentially cause serious injury and permanent harm, such as tissue necrosis.
- Injecting into the wrong tissue - Some substances need to be injected into certain types of tissue in order to be effective. For example, heroin is most potent when IV'd and can be extremely harmful when injected into the subcutaneous tissue. Ketamine, however, is typically IM'd. It is vital to ensure that one's hypodermic needle is correctly inserted into the vein before proceeding with an I.V injection.
Substances that are dangerous to inject
- Substances: See List of psychoactive substances to avoid#Contraindicated substances for injection
- Increased risk of overdose - This risk is especially present with opiates such as heroin. If one is injecting opiates, it is important to have naloxone available, if possible, as this can reverse the effects of an opiate drug overdose if administered quickly.[13] The risk of fatal overdoses rise sharply after a period of cessation and relapse, largely because of reduced tolerance.[14] To account for this lack of tolerance, it is safer to only dose a small fraction of one's usual dosage if relapsing after an extended break. It has also been found that the environment one is in can play a role fatal overdosing. In one scientific study, rats were significantly more likely to die after receiving their dose in an environment not associated with the drug in contrast to a familiar environment.[15] Other drugs are conditionally intramuscularly self-injected to prevent intravenous complications that can be prevented in a hospital setting. For example, ketamine taken intravenously quicker than 1.5 minute can cause breathing depression for short time (up to a minute).[16]
Dosage forms not intended for injection
See List of psychoactive substances to avoid#Dosage forms
Virus survival time outside the body
Survival time for dried viruses:
- Hepatitis B virus (HBV): 7 days[17]
- Hepatitis C virus (HCV): 6 weeks.[2]
- HIV: 7 days[2]
Materials and equipment
- A friend, and antidote - If possible, do your best not to IV/IM alone due to its high risk. The risk of overdose is significantly increased when injecting and having someone there to call the emergency services or give you medical aid (such as naloxone if an opioid is injected), can literally be the difference between life and death.
- Milligram scale - It is vital to weigh out the substance one is going to inject to help mitigate the risk of overdose.
- Alcohol swabs - This is for sterilization before and after injection. Hydrogen peroxide or other disinfectants can also be used.
- Soap - One should always wash their hands with soap and water before injecting. If soap and water are not available, alcohol-based hand sanitizer may be used, however, washing one's hands with soap and water is always preferable.
- Micron filters or cotton filters - These are used for cold water extraction, to filter out solid impurities in the substance solution. A cotton filter is better than nothing, but a micron filter is considered to be the best. If one is using a cotton filter it is important to never re-use this cotton filter as it can harbor bacteria and cause severe health consequences known as "cotton fever,"[18] that are releasing an endotoxin. This is due to the bacteria that grow in the moist conditions of the cotton filter - one should always dispose of their filters after a single use.
- pH regulation
- Vitamin C (ascorbic acid) - Useful for substances with high pH like crack (free base form may be too basic to be suitable for injection)[19]. Also, a weak acid can be added to heroin, and cocaine solutions to dissolve them from impurities more easily. It is important that one does not use fruit juice or vinegar as these lead to greater risks of infection. Vitamin C powder can be found in packets online. Too much vitamin C will make the solution too acidic and can cause vein problems.[20]
- Baking soda - Useful for substances with low pH.
- pH indicator - Especially useful if acid or bases are used.
- Elastic tourniquets or stockings - These can be used to "tie off", or make the veins more visible and accessible, during IV injection. These materials are better for skin than leather belts or other similar objects used to "tie off". Neckties, lubricated condoms, and socks can also be used. One should always use a slip knot when tying off so the tourniquet can be removed quickly if needed. The tourniquet should be removed immediately if there is a loss of sensation in the limbs or the limb discolors or turns blue.
Sterile water for injection

Sterile water for injection (sometimes abbreviated SWFI) is standardized ultrapure water used to create solutions that will be administered by injection. Water for injection is generally made by distillation or reverse osmosis.[21][22] Water for injection can also be used for nasal sprays, and eye drops.
Pharmacopoeia specifications for water for injection
| Properties | European Pharmacopoeia (Ph.Eur.)[23] | United States Pharmacopeia (USP)[24] |
|---|---|---|
| Conductivity | <1.3 μS/cm at 25 °C | <1.3 μS/cm at 25 °C |
| Total organic carbon (TOC) | <0.5 mg/L | <0.5 mg/L |
| Bacteria (guideline) | <10 CFU/100 mL | <10 CFU/100 mL |
| Endotoxin | <0.25 IU/mL | <0.25 EU/mL |
| Nitrates | <0.2 ppm | N/A |
| Aluminium | <10 ppb | N/A |
- If in-line conductivity exceeds values additional testing is required before a conclusion can be made. Refer to the respective pharmacopoeia for details.
- One USP Endotoxin Unit (EU) is equal to one International Unit (IU) of endotoxin
Other water sources
- Boiled tap water: It is also important to change the water at a regular interval to prevent bacteria growth within the water. Be mindful that using multiple hypodermic needles in the same water supply can easily spread illness and disease. No other liquid substance should be added to the injection, even if it is supposed to increase the solubility of the drug in the water solution. Heat can be used to aid dissolution, but fruit juice or vinegar can lead to infections. Hot tap water should always be avoided because it contains heavy metals.
- Eye drops
- Eye drops with medications (e.g. the deliriant tropicamide only used for ocular administration) can be deadly when injected.
- Syringe designed saline drops (e.g. Wallace Cameron Ultra Saline Minipod) are distributed in modern needle-exchange programmes as they can be used efficiently either by injection or ophthalmic (if the drug is potent in small doses) route of administer which is compared to intravenous use; by demonstration, the elimination of latanoprost acid from plasma is rapid (half-life 17 minutes) after either ophthalmic or intravenous administration.[25]
- Distilled water should be avoided in large amounts directly into a vein, as it can cause your blood cells to become hypotonic, possibly leading to death. Distilled water is often sold as battery water, but since it's not designed for medical use, it may lack specifications and may be unsafe to inject.
Sterile single-use spoon
"Do not put your needle into a common pool with others. This practice may be responsible for the spread of hepatitis C in people who say that they don't share needles."[26]
Typically, a small disposable aluminum single-use spoon, ideally color-coded, specifically designed for the purpose of dissolving and sterilizing the substance for injection.
In situations where people inject drugs, there's a chance of unknowingly sharing equipment like spoons, shot glasses, or even the concave bottom of a soda can. This can happen for several reasons:
- Incomplete sterilization: Washing with dish soap doesn't guarantee sterility. Used equipment might be put back for reuse by others, creating a risk of bloodborne disease transmission.
- Memory lapses: People may forget that the equipment was previously used and unintentionally share it, putting themselves and others at risk.
Sterile syringe and sterile hypodermic needle
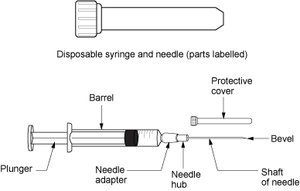
About 0.1 mL of the solution is lost in conventional syringes through the Luer taper tip and the Luer taper adapter of the hypodermic needle. That can be compensated by either adding extra 10% or 5% substance in 1 mL or 2 mL syringes respectively, or by using low dead space syringes.
Color coded syringes, hypodermic needles, and single-use spoons (also shared by needle and syringe programmes), are can help people under the influence to avoid sharing tools by mistake. Some people are marking the syringe with a marker pen, or colored tape.
Thinner hypodermic needles cause smaller wounds and scars.
Sterile syringe with sterile intravenous hypodermic needle
Used for IV injection. Insulin syringes (with cemented hypodermic needles) are common, but 1-2 mL syringes with short hypodermic needles (0.5 inch (13 mm), and 14-30 G) are also used (e.g. "tuberculin syringes"), meant to penetrate surface veins.
Drug users typically use a 25 g rapid (5-16 seconds) intravenous injection by arm via the median cubital vein to get a rush. However, smaller gauges such as 30 g can be used to prevent a vein collapse for repeated administration. Hypodermic needles smaller than 30 G are normally used for subcutaneous injection, but not for intravenous (coagulated blood immediately after blood response) or intramuscular use (the finest hypodermic needles are very short).
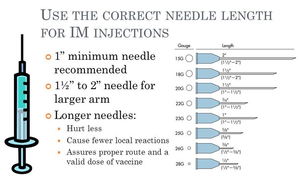
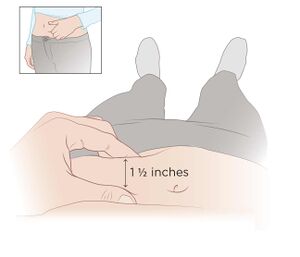
Sterile syringe with sterile intramuscular hypodermic needle
This type of syringe is used for the less common intramuscular (IM) injection. The syringes are typically 1 mL to prevent slow injection, and the hypodermic needles typically has a hole size of 22-25G, and are typically 1- to 1.5-inch (25–38 mm, and up to 3 inch (76 mm) for large adults) depending on body weight, which is longer than the traditional insulin needles seen for IV use because it is designed to penetrate deep into the muscular tissue instead of a vein.
"It is common to have muscle pain when injecting larger doses of liquid Ketamine into muscle tissue. The pain can continue for several days if it is not administered properly. The muscle soreness can be somewhat controlled by using a very fine (small gauge) needle and by injecting very slowly. It should take 15-30 or more seconds to inject a dose into a muscle. If you feel it begin to sting, slow down the injection rate."[27]
Naloxone
If injecting an opioid, it is highly recommended to carry naloxone if it is available. Naloxone is a substance used to reverse the effects of opioids in an overdose. Many jurisdictions have programs to distribute naloxone for free or at discount prices to people who are in need of it. Naloxone may be available as a nasal spray under the brand name "Narcan" or as an autoinjector with voice instructions.
Procedure
From the standpoint of harm reduction, all injection drug use is strongly discouraged because it maximizes harm potential while reducing the user's ability to use substances in a sustainable manner. It should be noted that intravenous injection is the most common form and is observed with opiates (e.g. heroin) and stimulants (e.g. cocaine and methamphetamine). Intramuscular administration is mostly observed with ketamine.
It is extremely important to vary the administration sites of injections. The overuse of one particular injection site can lead to degradation of the tissue of the site. With IV use, this can lead to collapsed veins.[28] Once a vein has collapsed, it cannot be used again. In regard to IM injection use, there have been animal studies that show there is risk of permanent scarring and damage the peripheral veins and muscle tissue if the site is overused.[29]
Solution for injection
Sterile water for injection (SWFI) should be placed in a single-use spoon when substances for injection are dissolved, in order to avoid spreading blood-borne diseases.
IV injection
- Administration sites - The most common administration site for an IV injection is in the body-facing side of the elbow, into the veins in the arm. The practice of injecting into extremities such as the hands, the feet, the legs, or even the pelvic area can lead to serious complications and bodily harm. The most dangerous places to inject are into the groin, the hands & feet, and the jugular veins in the neck. Injecting into the groin area is especially risky due to the femoral vein's location next to the femoral nerve and artery. The neck is the riskiest area to inject into because the jugular veins lie very close to the carotid artery, which can be fatal if injected into. Damaging the jugular veins can interfere with blood circulation to the brain. Also, veins in the legs are more likely than those in the arm to develop clots that can obstruct circulation and eventually break off and lodge in the lungs or heart, causing fatal bodily harm.
Dangers specific to IV drug use
- Cotton fever - A medical condition that indicates as a fever that follows intravenous drug use where cotton is used to filter the drugs.[31] The condition derives from an endotoxin released by the bacteria Pantoea agglomerans which lives in cotton plants.[32]
- Collapsed vein - Collapsed veins may never recover.
- Pulmonary embolism (PE) - Embolization of air, fat, and talc in the drugs is responsible for a small proportion of PE of people who inject substances.
- Thrombosis - After prolonged injection, thrombosis in the veins can occur. Thrombosis occurs when a vein’s blood flow is increasingly disrupted, creating blood clots in the lining of the vein. Eventually, the vein can become completely blocked by these clots, transforming the peripheral veins into scar tissue. This is commonly referred to as a collapsed vein.[10] To avoid this issue, the injection site should be rotated.
- Phlebitis (inflammation of a vein)
- Development of peripheral veins scar tissue - One should always inject the substance towards the heart, not away from it. By injecting with the flow of blood you may avoid problems caused by creating scar tissue or clots which occur when injecting against the flow of blood in the veins [33]. If the substance flows towards against the heart, instead of away from it, it may lead to increased scar tissue and risk of infection.
Procedure
- Clean your hands: Wash the hands with soap and water for 15-20 seconds.[34]
- Optionally: After you have washed your hands, use a hand sanitizer for 15 seconds.[35]
- Mix the chosen substance in sterile water for injection in a sterile single-use spoon, being careful not to exceed the amount of water that the syringe can hold.
- Boil the solution with a lighter for a few seconds.
- Let the solution cool down to room temperature.
- Suck up the solution into the syringe through the filter. Make sure that no big particles have escaped the filtration, even "pure" substances may have one or two dust particles, and injecting them intravenously can be really painful, which may also escalate a bad trip.
- Make sure no air bubbles are present in the reservoir before the plunger is released. Hold the syringe vertically and flick it with your fingers to release bubbles to the needle adapter, and gently push the plunger. Don't worry about air embolism, it is estimated that a large volume of 50-500 mL or greater infused at a rapid rate is potentially fatal.[36][37]
- Attach a fresh needle to the syringe.
- Prepare the injection site with an alcohol swab.
- Remove the needle cap.
- If using the traditional crook of the elbow injection site, one may need to apply pressure above the vein to make the vein stick out more. This is typically achieved through "tying off," which refers to the practice of wrapping a solid band or tourniquet around the upper forearm so that blood constricts and the veins become more visible.
- Take three deep breaths.
- The hypodermic needle will most likely have a bevel. It is important to angle the beveled edge away from the skin, so the point of the needle penetrates the vein and injects.
- Venipuncture: However, for typical injection in the arm, penetrate the skin at a 15 to 35-degree angle and always inject toward the heart. Avoid to push the hypodermic needle deeply into the vein to avoid extravasation which can serious injury and permanent harm, such as tissue necrosis.
- Once you have penetrated the skin, and it feels that you have punctured the vein with the hypodermic needle: Pull back on the plunger of the syringe, or hold the syringe vertically, so the blood can flow into it. If there is blood present in the syringe, the needle has hit a vein, and it is good to inject. If there is no blood in the syringe barrel or one feels a suck back, the needle is not in a vein; it is in subcutaneous tissue, so do NOT inject! Repeat the former venipuncture steps until the needle hits a vein.
- Once the hypodermic needle is in the vein, push the plunger down GRADUALLY for at least 30 seconds. It is highly advised not to rush the injection, especially if one is IVing a strong opiate, such as heroin. However, leaving the needle in the vein for a long time can cause it to be irritated.
- Once all the solutions have been injected, slowly remove the hypodermic needle.
- Block the bleeding from the vein by gently pushing a piece of toilet paper on it for approximately 20 seconds.
- Use a new alcohol swab to clean the injection site. There may be a little blood.
Foot injection
For self-administration it is often easier, especially for people with a high percentage of body fat, to inject a great saphenous vein in a foot rather than the median cubital vein by arm. Also, wounds in the feet might look less suspicious and are easy to cover with socks. A foot bath will enlarge the veins.
IM injection
- Administration sites - Common injection sites for intramuscular injections include the buttocks, the arm, and the thigh.[38]
- Hypodermic needle length - It is important that one uses a hypodermic needle that is longer than the IV needle in order to reach the muscle tissue.
- Clean your hands: Wash the hands with soap and water for 15-20 seconds.[39]
- Optionally: After you have washed your hands, use a hand sanitizer for 15 seconds.[40]
- Mix the chosen substance in sterile water for injection in a sterile single-use spoon, being careful not to exceed the amount of water that the syringe can hold.
- Boil the solution with a lighter for a few seconds.
- Let the solution cool down to room temperature.
- Suck up the solution into the syringe through the filter. Make sure that no big particles have escaped the filtration, even "pure" substances may have one or two dust particles, and injecting them intravenously can be really painful, which may also escalate a bad trip.
- Make sure no air bubbles are present in the reservoir before the plunger is released. Hold the syringe vertically and flick it with your fingers to release bubbles to the needle adapter, and gently push the plunger. Don't worry about air embolism, it is estimated that a large volume of 50-500 mL or greater infused at a rapid rate is potentially fatal.[41][42]
- Attach a fresh needle to the syringe.
- Prepare the injection site with an alcohol swab.
- Remove the needle cap.
- To prepare the hypodermic needle, hold the syringe with the dominant hand and pull the cover off with the other hand. Place the syringe between the thumb and first finger.
- Hold the skin around where the injection will be administered. With the free hand, gently press on and pull the skin so that it is slightly tight.
- Hold the syringe barrel tightly and use the wrist to inject the hypodermic needle through the skin and into the muscle at a 90-degree angle.
- Let go of the skin with the other hand. Hold the syringe, so it stays pointed straight in. Pull back on the plunger a little to make sure the hypodermic needle did not hit a blood vessel. The point of intramuscular injection is to inject within the muscle itself. If blood comes back into the syringe barrel, remove the needle immediately and do not inject. If possible, dispose of the needle and syringe and get a new one. When giving the second injection, use a different injection site than the first.
- Push down on the plunger to inject the solution. Do not push the plunger down hard and fast; some substance solutions may burn. Injecting at a slower rate reduces the pain.
- Once the solution is injected, remove the hypodermic needle at the same angle as it went in. Re-swab the area of injection with an alcohol swab.
SC injection
Warning: This method of injection is uncommon and is not advised. The hypodermic needle may break off in the skin, hit a nerve, or cause scarring, lumps, and other skin problems. Additionally, the risks of infection are greatly increased when using this method of administration.
- Hypodermic needle type - An IV or insulin hypodermic needle length is suitable for this type of injection. Do not use a longer needle length as it can penetrate other types of tissue and cause medical problems.
- Administration sites - The areas where SC injections can be administered in are the abdomen, the thigh, the lower back, and the upper arm.[43] It is important to vary the injection site to avoid infections or injuries. Seek immediate medical care if a rash develops at the injection site or swelling is present after injecting.
- Clean your hands: Wash the hands with soap and water for 15-20 seconds.[44]
- Optionally: After you have washed your hands, use a hand sanitizer for 15 seconds.[45]
- Mix the chosen substance in sterile water for injection in a sterile single-use spoon, being careful not to exceed the amount of water that the syringe can hold.
- Boil the solution with a lighter for a few seconds.
- Let the solution cool down to room temperature.
- Suck up the solution into the syringe through the filter. Make sure that no big particles have escaped the filtration, even "pure" substances may have one or two dust particles, and injecting them intravenously can be really painful, which may also escalate a bad trip.
- Make sure no air bubbles are present in the reservoir before the plunger is released. Hold the syringe vertically and flick it with your fingers to release bubbles to the needle adapter, and gently push the plunger. Don't worry about air embolism, it is estimated that a large volume of 50-500 mL or greater infused at a rapid rate is potentially fatal.[46][47]
- Attach a fresh needle to the syringe.
- Prepare the injection site with an alcohol swab.
- Remove the needle cap.
- Hold the syringe in the dominant hand and grasp and pinch the skin where one will administer the SC injection.
- Insert the hypodermic needle into the skin and slightly pull the plunger back. No blood should enter the syringe barrel to ensure that you are in subcutaneous tissue.
- Slowly inject the substance into the subcutaneous tissue.
- Remove the hypodermic needle at the same angle that it entered and re-wipe the injection site with an alcohol wipe.
Cleaning up after injection
In order to prevent the spread of blood-borne diseases and bacterial infections, clean up and dispose of used hypodermic needles and syringe barrels properly. The needle and barrel of the syringe can hold old blood, that can harbor viruses.
Single-use spoons
Single-use spoons are made of thin metal sheets, which make them easy to press together to indicate that they have been used.
Hypodermic needles
One should always re-cap their own old hypodermic needle after injection to ensure that other people are not exposed to the old blood that still resides in the needle. The needle can and will cause accidental skin pricks that transmit disease. Do not let others re-cap someone's own used needle!
After the needle has been re-capped, it should be disposed of properly. Take the used needle and syringe to a medical waste/sharps disposal facility near you. Do not simply leave the needles lying around as this makes them available for re-use by others and is a possible vector for disease. Leaving needles lying around, especially if they are uncapped, also leads to an increased risk of accidental skin pricking which can cause injury, infection, or disease.
Syringes
After you have attached the cap to the hypodermic needle, make sure that the needle is still fully attached to the syringe adapter, and discard them in a sharps disposal container. If you don't own a sharps disposal container, you can carefully bend thin 1 mL plastic syringes (with the plunger fully attached) 90 degrees, to prevent anyone from re-using them.
Medicine bags
If there are residues of injection fluid left in the syringe, it is considered medical waste. Then put the needle-free syringe in a pharmacy's plastic medicine bag. The same applies to ampules with residual injection fluid.
Sharps disposal containers
You'll find sharps disposal containers in your local drug store, often offered gratis. They are also offered in needle exchange programs.
However, if you don't have access to a sharps disposal container, please collect the syringes and hypodermic needles in a puncture and leak-resistant plastic container, and leave it to your drug store as soon as possible.
Biological residues
Don't flush residues from the hypodermic needle and syringe in a glass of water and leave publicity available. Blood residues can fool someone to think it's actually squash and drink from it (yes, for real). Also, glass or other containers, contaminated with blood, can cause blood-borne diseases when used by others. It's safer to flush the syringe and needle under an interior water tap in the sink, as long as they don't get in touch with it.
Aftercare
The injection site should be monitored for swelling, redness, or any other signs of infection. Seek medical attention from a doctor if you think the injection site may be infected or an abscess forms. An abscess may appear red, filled with puss, and hard and it may be a sign of a potentially serious infection. Seek medical care immediately if persisting discomfort is experienced.
- Getting tested - Regular STD tests and hepatitis B & C tests should be performed, especially if one suspects that they have injected with contaminated materials or has shared injection materials with others. Anonymous STD tests can be performed at local clinics or national organizations like Planned Parenthood.[48]
- Proper vein care - One should avoid using veins that are tender, hardened, or inflamed until these veins have healed. It is important to take care of past injection sites, monitor them for signs of infection, and vary current injection sites.
- Shooting into the wrong tissue - If one misses an IV injection, it is important that the area is treated with a warm water soak or compress to reduce the likelihood of irritation and abscess formation. Warmth will open the capillaries and bring disease-fighting white blood cells to the affected area.
Sterilization of re-used equipment
Equipment that never should be re-used
Cotton is often used for filtration. However, cotton fever is a condition derives from an endotoxin released by the bacteria Pantoea agglomerans.
An autoclave is required to sterilize equipment
Glass syringes, and single-use spoons, can be sterilized with an autoclave. It's not advised to sterilize solid metal hypodermic needles that have been used, because their needle points are blunt.
Sterilizing capacity of an autoclave:
- Hepatisis C virus (HCV): Sterilizing hypodermic needles using bleach, boiling water or alcohol may not kill HCV.[49] So it is not advised to share cooking pans to sterilizing equipment.
Sterilizing capacity of an autoclave or pressure cooker:
- Prion: "For prion elimination, various recommendations state 121–132 °C (250–270 °F) for 60 minutes or 134 °C (273 °F) for at least 18 minutes."[50] A pressure cooker reach 120 °C at full pressure.
Legality
The injection of illegal drugs may lead to a higher risk of legal consequences. These consequences differ by country, state, and county. One should research the laws in their region before choosing to inject.
- Hypodermic needles and syringes - Hypodermic needles and syringes are illegal to possess without a prescription in some states,[51] and countries.
- Overdoses - If someone overdoses, the person who stays with them and calls emergency medical services will not be prosecuted. Do not simply leave a person who has overdosed to die out of fear of legal repercussions. The legal repercussions of staying with someone that has experienced drug overdose and calling emergency medical services vary by location.
- In the United States, the states that have "good samaritan" laws (in varying degrees) protecting those that call EMS as of January 2016 are: Alabama, Alaska, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Kentucky, Louisiana, Maryland, Massachusetts, Minnesota, Mississippi, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Oregon, Pennsylvania, Rhode Island, Tennessee, Vermont, Washington State, West Virginia, and Wisconsin.[52]
- Naloxone - This life-saving drug is illegal to possess in some states, counties, or countries. Throughout the world, naloxone is not considered a controlled substance. In most countries, it is a prescription drug.
- Australia: In Australia, naloxone is considered an over the counter drug and is available at most pharmacies.[53]
- Canada: In Canada, naloxone kits are distributed in many emergency rooms and clinics.
- United States: At a federal level in the USA, naloxone is a prescription drug. Many states have programs that make naloxone over the counter and available at request at most pharmacies. In the United States, most jurisdictions have programs to deploy naloxone to law enforcement and fire and rescue services. The states that have a naloxone access laws (in varying degrees) as of January 2016 are: Alabama, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Illinois, Kentucky, Louisiana, Maryland, Massachusetts, Minnesota, Michigan, Mississippi, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington State, West Virginia, and Wisconsin.[54]
- United Kingdom: In the United Kingdom, naloxone is considered a Prescription Only Medicine. It is also given out at drug intervention programs and needle distribution centers, provided one has undertaken a quick 10 minute training protocol.
Substance notes
Drugs that are useless to inject
- Lisdexamfetamine dimesylate (Vyvanse) - is formulated with a low potential for abuse as it is a prodrug necessitating conversion to dextroamphetamine in the gastrointestinal tract or liver.
Drugs that require special consideration to inject
- Some psychoactive substances such as benzodiazepines (valium, oxazepam, clonazepam) are water soluble to a small degree (about 3.5ml/mg).
See also
External links
- Drug injection (Wikipedia)
- Hardware Vault Syringe & Needle Basics (Erowid)
- Injecting Advice – A website for harm reduction workers and people who inject drugs
- Getting Off Right Safety Manual (Harmreduction.org)
- Safer Injecting Guide.pdf (Drugs.ie)
- lawatlas.org - provides needle access information on a state by state basis
- Fact Sheet States With Naloxone Access and Good Samaritan Laws for 2016
References
- ↑ https://www.cdc.gov/hepatitis/hcv/pdfs/factsheet-pwid.pdf
- ↑ 2.0 2.1 2.2 Paintsil, E; Binka, M; Patel, A; Lindenbach, BD; Heimer, R (15 April 2014). "Hepatitis C virus maintains infectivity for weeks after drying on inanimate surfaces at room temperature: implications for risks of transmission". The Journal of infectious diseases. 209 (8): 1205–11. doi:10.1093/infdis/jit648. PMC 3969546
 . PMID 24273176.
. PMID 24273176.
- ↑ Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L (August 2011). "Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews". Lancet. 378 (9791): 571–83. doi:10.1016/S0140-6736(11)61097-0. PMC 3285467
 . PMID 21802134.
. PMID 21802134.
- ↑ Xia X, Luo J, Bai J, Yu R (October 2008). "Epidemiology of hepatitis C virus infection among injection drug users in China: systematic review and meta-analysis". Public Health. 122 (10): 990–1003. doi:10.1016/j.puhe.2008.01.014. PMID 18486955.
- ↑ Editor (2011), Bioavailability of Drugs
- ↑ Evans, S. M., Cone, E. J., Henningfield, J. E. (1 December 1996). "Arterial and venous cocaine plasma concentrations in humans: relationship to route of administration, cardiovascular effects and subjective effects". Journal of Pharmacology and Experimental Therapeutics. 279 (3): 1345–1356. ISSN 0022-3565.
- ↑ 7.0 7.1 What should I do if I injure myself with a used needle?, 2018
- ↑ Skin infections in intravenous drug users, DermNet NZ
- ↑ Gaspar, M. R., Hare, R. R. (October 1972). "Gangrene due to intra-arterial injection of drugs by drug addicts". Surgery. 72 (4): 573–577. ISSN 0039-6060.
- ↑ 10.0 10.1 10.2 IV Injection Sites - Potentially Deadly Spots to Shoot Up, 2015
- ↑ Deep Vein Thrombosis (DVT) Symptoms, Treatment, Causes, Diagnosis
- ↑ Cornford, C. S., Mason, J. M., Inns, F. (December 2011). "Deep vein thromboses in users of opioid drugs: incidence, prevalence, and risk factors". The British Journal of General Practice. 61 (593): e781–e786. doi:10.3399/bjgp11X613115. ISSN 0960-1643.
- ↑ Overdose Prevention For Injection Drug Users (drugpolicy.org) | http://www.drugpolicy.org/resource/overdose-prevention-injection-drug-users
- ↑ Why Heroin Relapse Often Ends In Death - Lauren F Friedman (Business Insider) | http://www.businessinsider.com.au/philip-seymour-hoffman-overdose-2014-2
- ↑ Siegel, S., Hinson, R. E., Krank, M. D., McCully, J. (23 April 1982). "Heroin "Overdose" Death: Contribution of Drug-Associated Environmental Cues". Science. 216 (4544): 436–437. doi:10.1126/science.7200260. ISSN 0036-8075.
- ↑ Ketamine: Dreams and Realities, p276
- ↑ https://www.cdc.gov/hepatitis/hbv/bfaq.htm
- ↑ (PDF) http://heroinhelper.com/pdf/heroin-helper.pdf. Missing or empty
|title=(help) - ↑ "Ask Erowid : ID 2854 : What form does 5-MeO-DMT have to be in to be smoked?". www.erowid.org.
- ↑ Safer injection (catie.ca) | http://www.catie.ca/en/practical-guides/hepc-in-depth/prevention-harm-reduction/safer-injection
- ↑ https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/018632s051lbl.pdf
- ↑ Ghosh, Tapash K.; Jasti, Bhaskara R. (2004). Theory and Practice of Contemporary Pharmaceutics (in English). CRC Press. p. 396. ISBN 9780203644478. Archived from the original on 2017-01-16. Unknown parameter
|url-status=ignored (help) - ↑ "Water for injections". European Pharmacopoeia (in English) (8 ed.). Strasbourg, France: Council of Europe. 2013. pp. 3555–3558. ISBN 978-92-871-7531-1.
- ↑ "USP Monographs: Water for Injection". United States Pharmacopeia and the National Formulary (USP-NF) (USP38–NF33 ed.). Rockville, MD, USA: U.S. Pharmacopeial Convention. October 2014. p. 5805.
- ↑ "Latanoprost Drug Information, Professional". Drugs.com. Retrieved 18 September 2014.
- ↑ [Ketamine: Dreams and Realities, p269]
- ↑ "Erowid Ketamine Vault : Dosage". www.erowid.org.
- ↑ http://new.sfaf.org/tspsf/speedometer/shooters/vein_care.html
- ↑ Diness, V. (May 1985). "Local tissue damage after intramuscular injections in rabbits and pigs: quantitation by determination of creatine kinase activity at injection sites". Acta Pharmacologica Et Toxicologica. 56 (5): 410–415. doi:10.1111/j.1600-0773.1985.tb01311.x. ISSN 0001-6683.
- ↑ 30.0 30.1 Getting Off Right (Safety Manual)
- ↑ Harrison, D. W.; Walls, R. M. (April 1990). ""Cotton fever": a benign febrile syndrome in intravenous drug abusers". The Journal of Emergency Medicine. 8 (2): 135–139. doi:10.1016/0736-4679(90)90222-H. ISSN 0736-4679. PMID 2362114.
- ↑ Ferguson, R. (1993-10-25). "Enterobacter agglomerans--associated cotton fever". Archives of Internal Medicine. 153 (20): 2381–2382. doi:10.1001/archinte.153.20.2381. ISSN 0003-9926. PMID 8215743.
- ↑ Brunsdon, N. (2018), Better Vein Care Guide
- ↑ Toney-Butler, Tammy J.; Gasner, Adi; Carver, Niki (2022). "Hand Hygiene". StatPearls. StatPearls Publishing.
- ↑ Pires, D; Soule, H; Bellissimo-Rodrigues, F; Gayet-Ageron, A; Pittet, D (May 2017). "Hand Hygiene With Alcohol-Based Hand Rub: How Long Is Long Enough?". Infection control and hospital epidemiology. 38 (5): 547–552. doi:10.1017/ice.2017.25. PMID 28264743.
- ↑ http://www.ajol.info/index.php/sajr/article/viewFile/34461/6388. Missing or empty
|title=(help) - ↑ Gordy S, Rowell S (January 2013). "Vascular air embolism". International Journal of Critical Illness and Injury Science. 3 (1): 73–76. doi:10.4103/2229-5151.109428. PMC 3665124
 . PMID 23724390.
. PMID 23724390.
- ↑ Intramuscular Injection, 2022
- ↑ Toney-Butler, Tammy J.; Gasner, Adi; Carver, Niki (2022). "Hand Hygiene". StatPearls. StatPearls Publishing.
- ↑ Pires, D; Soule, H; Bellissimo-Rodrigues, F; Gayet-Ageron, A; Pittet, D (May 2017). "Hand Hygiene With Alcohol-Based Hand Rub: How Long Is Long Enough?". Infection control and hospital epidemiology. 38 (5): 547–552. doi:10.1017/ice.2017.25. PMID 28264743.
- ↑ http://www.ajol.info/index.php/sajr/article/viewFile/34461/6388. Missing or empty
|title=(help) - ↑ Gordy S, Rowell S (January 2013). "Vascular air embolism". International Journal of Critical Illness and Injury Science. 3 (1): 73–76. doi:10.4103/2229-5151.109428. PMC 3665124
 . PMID 23724390.
. PMID 23724390.
- ↑ How To Give A Subcutaneous Injection (drugs.com) | https://www.drugs.com/cg/how-to-give-a-subcutaneous-injection.html/
- ↑ Toney-Butler, Tammy J.; Gasner, Adi; Carver, Niki (2022). "Hand Hygiene". StatPearls. StatPearls Publishing.
- ↑ Pires, D; Soule, H; Bellissimo-Rodrigues, F; Gayet-Ageron, A; Pittet, D (May 2017). "Hand Hygiene With Alcohol-Based Hand Rub: How Long Is Long Enough?". Infection control and hospital epidemiology. 38 (5): 547–552. doi:10.1017/ice.2017.25. PMID 28264743.
- ↑ http://www.ajol.info/index.php/sajr/article/viewFile/34461/6388. Missing or empty
|title=(help) - ↑ Gordy S, Rowell S (January 2013). "Vascular air embolism". International Journal of Critical Illness and Injury Science. 3 (1): 73–76. doi:10.4103/2229-5151.109428. PMC 3665124
 . PMID 23724390.
. PMID 23724390.
- ↑ STD Testing Procedure - Facts About STD Screening & Tests
- ↑ Mukherjee, TI; Pillai, V; Ali, SH; Altice, FL; Kamarulzaman, A; Wickersham, JA. doi:10.1016/j.drugpo.2017.05.041. PMC 5592150
 . PMID 28652072 //www.ncbi.nlm.nih.gov/pmc/articles/PMC5592150. Missing or empty
. PMID 28652072 //www.ncbi.nlm.nih.gov/pmc/articles/PMC5592150. Missing or empty |title=(help) - ↑ Rutala, WA; Weber, DJ; Society for Healthcare Epidemiology of, America (February 2010). "Guideline for disinfection and sterilization of prion-contaminated medical instruments". Infection control and hospital epidemiology. 31 (2): 107–17. doi:10.1086/650197. PMID 20055640.
- ↑ Syringe Distribution Laws
- ↑ State Good Samaritan Laws in the USA | http://www.drugpolicy.org/sites/default/files/Fact%20Sheet_State%20based%20Overdose%20Prevention%20Legislation%20%28January%202016%29.pdf
- ↑ How painkiller use becomes a heroin addiction, 2016
- ↑ State Naloxone Laws in the USA http://www.drugpolicy.org/sites/default/files/Fact%20Sheet_State%20based%20Overdose%20Prevention%20Legislation%20%28January%202016%29.pdf