Cannabinoid


A cannabinoid is one of a class of diverse chemical compounds that act on cannabinoid receptors on cells that alter neurotransmitter functioning in the brain. These receptor proteins include the endocannabinoids (produced naturally in the body by humans and animals),[1] the phytocannabinoids (found in cannabis and some other plants), and synthetic cannabinoids (manufactured chemically).
The most notable cannabinoid is the phytocannabinoid ∆9-tetrahydrocannabinol (THC), the primary psychoactive compound of cannabis.[2][3] Cannabidiol (CBD) is another major constituent of the plant, representing up to 40% in extracts of the plant resin.[4] There are at least 85 different cannabinoids isolated from cannabis which exhibit varied effects.
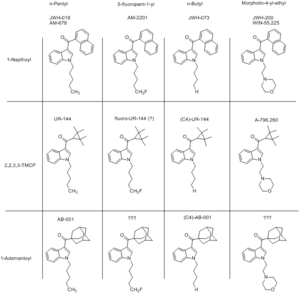
Synthetic cannabinoids encompass a variety of distinct chemical classes: the classical cannabinoids structurally related to THC; the nonclassical cannabinoids (cannabimimetics) including the aminoalkylindoles, 1,5-diarylpyrazoles, quinolines, and arylsulphonamides; and eicosanoids related to the endocannabinoids.[2][3]
Cannabinoid receptors
Before the 1980s, it was often speculated that cannabinoids produced their physiological and behavioral effects via nonspecific interactions instead of interacting with specific receptors directly. The discovery of the first cannabinoid receptors in the 1980s helped to resolve this debate. These receptors are common in animals and have been found in mammals, birds, fish, and reptiles. At present, there are two known types of cannabinoid receptors, termed CB1 and CB2,[1] with mounting evidence of more.[5][6] However, the role of these interactions and how they result in the cannabinoid high experience continues to remain elusive.
Cannabinoid receptor type 1
CB1 receptors are found primarily in the brain, more specifically in the basal ganglia and in the limbic system (including the hippocampus).[1] They are also found in the cerebellum and in both male and female reproductive systems. CB1 receptors are absent in the medulla oblongata, the part of the brain stem responsible for respiratory and cardiovascular functions. Thus, there is not the risk of respiratory or cardiovascular failure that can be produced by some drugs. CB1 receptors appear to be responsible for the euphoric and anticonvulsive effects of cannabis. However, the role of these interactions and how they result in the cannabinoid high experience continues to remain elusive.
Cannabinoid receptor type 2
CB2 receptors are predominantly found in the immune system, or immune-derived cells[7] with the greatest density in the spleen. While found only in the peripheral nervous system, a report does indicate that CB2 is expressed by a subpopulation of microglia in the human cerebellum.[8] CB2 receptors appear to be responsible for the anti-inflammatory and possibly other therapeutic effects of cannabis.[7] However, the role of these interactions and how they result in the cannabinoid high experience continues to remain elusive.
Subjective effects
Disclaimer: The effects listed below cite the Subjective Effect Index (SEI), an open research literature based on anecdotal user reports and the personal analyses of PsychonautWiki contributors. As a result, they should be viewed with a healthy degree of skepticism.
It is also worth noting that these effects will not necessarily occur in a predictable or reliable manner, although higher doses are more liable to induce the full spectrum of effects. Likewise, adverse effects become increasingly likely with higher doses and may include addiction, severe injury, or death ☠.
Physical effects 
-
- Sedation - Although certain strains of cannabinoids present mild encouraged stimulation at low to moderate doses, for the most part the effects on the user's energy levels are primarily sedating. This encourages one to relax, but can, however, be suppressed by simply forcing oneself to engage in physical activities.
- Motor control loss - These substances cause a partial to moderate suppression of motor control which intensifies proportional to dosage but rarely results in a complete inability to walk and perform basic movements.
- Appetite enhancement - The feeling of increased appetite following the use of cannabinoids has been documented for hundreds of years[9] and is known colloquially as "the munchies" in popular American and United Kingdom culture. Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food.[10] This is thought to be due to the way in which endocannabinoids in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake.
- Nausea suppression - Cannabis is effective for suppressing nausea induced by both general illness and substances. It is considered an effective treatment for chemotherapy-induced nausea and vomiting (CINV)[11] and is a reasonable option in those who do not improve following preferential treatment.[12]
- Dehydration
- Vasodilation - THC decreases blood pressure which dilates the blood vessels and increases blood flow throughout the body. The arteries in the eyeball expand from the decreased blood pressure. Studies in the 1970s showed marijuana, when smoked or eaten, effectively lowers intraocular pressure by about 25%, as much as standard medications.[13] These enlarged arteries often produce a bloodshot red eye effect. It is precisely this effect on the human eye that makes cannabinoids an effective medicine for glaucoma.[14]
- Pain relief - This substance has been reported as being useful for treating certain headaches and chronic pain, including pain caused by neuropathy and possibly fibromyalgia and rheumatoid arthritis.[15][16]
- Perception of increased weight or Perception of decreased weight - Depending on the specific cannabinoid, one can find themselves with a body which can feel either physically heavier or lighter than it usually would in a manner that is entirely dependent upon dosage.
- Changes in gravity - At extremely high doses, many users report a feeling of being pulled backwards across vast distances at powerful speeds. This sensation progressively increases in intensity and eventually becomes unbearable if one leans backwards or lies down but usually disappears altogether once the user sits up or leans forward.
- Spontaneous tactile sensations
Visual effects 
-
- Brightness alteration
- Colour enhancement
- Visual acuity suppression
- Geometry - Certain cannabinoids are capable of inconsistently inducing mild to intense psychedelic geometry at high doses. Within many users who also regularly use psychedelics, however, they are capable of inducing these consistently in a visual style which seems to be an averaged out depiction of all the psychedelics one has used within the past. These rarely extend beyond level 4 and are considered to be mild, fine, small and zoomed out (but often well-defined).
- Internal hallucinations
Cognitive effects 
-
- Anxiety - Certain cannabinoids induce anxiety consistently; however, all cannabinoids are capable of inducing anxiety at high doses or with chronic administration.
- Conceptual thinking
- Emotion enhancement - The most prominent cognitive component of the cannabinoid experience is the way in which it enhances the emotions one is already feeling proportional to dosage. This can result in euphoria, extreme laughter, and increased immersion within tasks and activities or it can result in anxiety or paranoia depending on the user's current state of mind.
- Feelings of impending doom
- Mindfulness
- Novelty enhancement - This effect is most notable when high levels of THCV are present.
- Increased music appreciation
- analysis suppression
- Paranoia - Certain cannabinoids induce paranoia consistently and all cannabinoids are capable of inducing paranoia at high doses or with chronic administration.
- Sleepiness
- Thought connectivity
- Thought deceleration
Auditory effects 
Phytocannabinoids
Phytocannabinoids can be defined as any plant-derived natural product capable of either directly interacting with cannabinoid receptors or sharing chemical similarity with cannabinoids or both. The entourage effect is a proposed mechanism by which compounds present in cannabis which are largely non-psychoactive by themselves modulate the overall psychoactive effects of the plant (these resulting principally from the action of the main psychoactive component of cannabis, tetrahydrocannabinol (THC)).
Phytocannabinoid ← phytocannabinoid acid
Quasi-psychedelic phytocannabinoids
- Δ-8-THC. Psychoactive, but about half as potent as Δ-9-THC.
- Decarboxylation: Δ-8-THCA → Δ-8-THC -- only trace amounts exist in cannabis
- Chemical conversion: CBD + acid 8 h → 50% Δ-8-THC
- Δ-9-THC (THC). Most abundant psychoactive component of cannabis. Is the standard when comparing THC analogs.
- Biosynthesis: Tetrahydrocannabinolic acid (THCA) synthase is an enzyme responsible for catalyzing the formation of THCA from cannabigerolic acid (CBGA). GMO yeast with a transgenic placement of a THCA synthase gene from Cannabis will produce THC
- Decarboxylation: THCA (more info) → THC -- The decarboxylation of this compound by heat is essential for the psychoactive effect of smoked cannabis, and depends on conversion of the enol to a keto group when the alpha carbon is protonated.
- Chemical conversion: CBD + acid 8 h → 50% THC
- Δ-10-THC. Psychoactive, but less potent than Δ-8-THC.
- Decarboxylation: Δ-10-THCA → Δ-10-THC-- only trace amounts exist in cannabis
- Chemical conversion: CBD + acid
- Δ-11-THC. Psychoactive, but little is known about this compound.
- THCB (more info)
- THCH (more info). 25 times more potent than THC.
- Decarboxylation: THCHA → THCH -- only trace amounts exist in cannabis
- Chemical conversion: CBDH + acid
- THCP (more info). 30 times more potent than THC.
- Biosynthesis: CBGPA → THCPA → THCP[17]
- Decarboxylation: THCPA → THCP-- only trace amounts exist in cannabis
- Chemical conversion: CBDP + acid
Quasi-psychedelic phytocannabinoids synthesized through chemical modification
- HHC
- HHCH
- HHCP-O-acetate
- THC-O-acetate. 3-5 times more potent than THC.
- Metabolization: THCAO is a prodrug, meaning it requires metabolization in order to take effect. It metabolically undergoes an activation process of converting to THC through de-acetylation, then THC continues into its own primary metabolites similarly to THC's oral route. Because of this, the onset when smoked can be significantly longer ranging from 20-45 minutes, but not as long as ingesting THC orally in comparison. THCAO through the oral route can also have longer onsets than oral THC due to its extra metabolic processes, with an onset of around 90 minutes.[18]
- Decarboxylation: Lack of information on decarboxylation, but it can be inferred that it decarboxylates like its normal parent compound since research suggests that heating it at 340°C (644°F) unbinds the acetyl group, releasing toxic ketene gas.[19]
- Chemical conversion: acetic anhydride + Δ-9-THC/Δ-8-THC → Δ-9-THCAO/Δ-8-THCAO, respectively.[20]
- THCP-O-acetate
Non-quasi-psychedelic phytocannabinoids, some which can be synthesized to quasi-psychedelic cannabinoids with biosynthesis or chemical conversion (see above)
- CBC ← CBCA
- CBCV ← CBCVA
- CBD
- Biosynthesis: CBGA → CBDA → CBD[21]
- Decarboxylation: CBDA → CBD
- Chemical conversion: THC + iodine → CBD
- CBDD
- CBDV ← CBDVA
- CBDH
- CBDP
- Biosynthesis: CBGPA → CBDPA → CBDP[22]
- Decarboxylation: CBDPA → CBDP
- CBE ← CBEA
- CBG
- CBGM ← CBGAM
- CBGV ← CBGVA
- CBL ← CBLA
- CBLV ← CBLVA
- CBN ← CBNA
- CBT ← CBTA
- CBV ← CBVA
- THCC ← THCCA
- Despite sounding a lot like THC, THCC is more similar to CBD than it is to THC
- THCV ← THCVA
- THCV is non-psychoactive.[23]
Plant sources
Synthetic cannabinoids
Synthetic cannabinoids are any artificial compound which is functionally similar to Δ9-tetrahydrocannabinol (THC), the active principle of cannabis. Like THC, they bind to the same cannabinoid receptors in the brain and are often sold as legal alternatives.
Toxicity and harm potential
Unlike cannabis, there have been multiple deaths[24][25][26][27][28][29][30] associated with the repeated abuse of synthetic cannabinoids as well as serious side effects resulting from its long-term use.[31][32][33] Therefore, it is strongly discouraged to take this substance for extended periods of time or in excessive doses. Compared to cannabis and its active cannabinoid THC, the adverse effects are often much more severe and can include high blood pressure, increased heart rate, heart attacks,[34][35] agitation,[36] vomiting,[37][38][39] hallucinations,[40] psychosis,[41][42][36][43] seizures,[44][45][46] and convulsions[47][48] as well as many others. Sixteen cases of acute kidney injury resulting from synthetic cannabinoid abuse have been reported.[49] JWH-018 has also been associated with strokes in two healthy adults.[50]
It should be noted that pre-mixed, branded blends (like Spice and K2) are more dangerous than pure powder because the specific chemicals and dosages are usually unlisted as well as the potential of inconsistent areas of dense powder, leading to an overdose. As synthetic cannabinoids are active in the milligram range (with below 5mg being a common dose), it is important to use proper precautions when dosing to avoid a negative experience.
Like THC, prolonged usage of synthetic cannabinoids may increase one's disposition to mental illness and psychosis[42], particularly in vulnerable individuals with risk factors for psychotic illnesses (like a past or family history of schizophrenia).[51][52][36] It is recommended that individuals with risk factors for psychotic disorders not use synthetic cannabinoids.[53]
Although there is no valid data on the toxicity of synthetic cannabinoids so far, there is concern that the naphthalene group found in THJ-018 and some other synthetic cannabinoids may be toxic or carcinogenic.[54][55][56][57]
It is strongly recommended that one use harm reduction practices when using these drugs.
Common substances
Brand-name mystery blends
Please be aware that pre-mixed, branded blends are unreliable as they often fail to list the constituents and dosages. Many people have been hospitalised or suffered negative symptoms believing they are comparable to cannabis in potency and effects. This is not the case, and they should be avoided in favour of pure analytical samples where possible.
Indazolecarboxamides
Indolecarboxamides
Indolecarboxylates
Naphthoylindoles
Naphthoylindazoles
Tetramethylcyclopropanoylindoles
Comprehensive List
For a comprehensive list of known synthetic cannabinoid derivatives, /r/Drugs/wiki has published a respectable directory of names and links to further information.
External links
References
- ↑ 1.0 1.1 1.2 Pacher, P., Bátkai, S., Kunos, G. (September 2006). "The endocannabinoid system as an emerging target of pharmacotherapy". Pharmacological Reviews. 58 (3): 389–462. doi:10.1124/pr.58.3.2. ISSN 0031-6997.
- ↑ 2.0 2.1 Lambert, D. M., Fowler, C. J. (11 August 2005). "The endocannabinoid system: drug targets, lead compounds, and potential therapeutic applications". Journal of Medicinal Chemistry. 48 (16): 5059–5087. doi:10.1021/jm058183t. ISSN 0022-2623.
- ↑ 3.0 3.1 Abood, M. E., Pertwee, R. G., eds. (2005). Cannabinoids. Handbook of experimental pharmacology. Springer. ISBN 9783540225652.
- ↑ UNODC - Bulletin on Narcotics - 1962 Issue 3 - 004
- ↑ Begg, M., Pacher, P., Batkai, S., Oseihyiaman, D., Offertaler, L., Mo, F., Liu, J., Kunos, G. (May 2005). "Evidence for novel cannabinoid receptors". Pharmacology & Therapeutics. 106 (2): 133–145. doi:10.1016/j.pharmthera.2004.11.005. ISSN 0163-7258.
- ↑ Boron, W. F., Boulpaep, E. L., eds. (2009). Medical physiology: a cellular and molecular approach (2nd ed., International ed ed.). Saunders/Elsevier. ISBN 9781416031154.
- ↑ 7.0 7.1 Pacher, P., Mechoulam, R. (April 2011). "Is lipid signaling through cannabinoid 2 receptors part of a protective system?". Progress in Lipid Research. 50 (2): 193–211. doi:10.1016/j.plipres.2011.01.001. ISSN 1873-2194.
- ↑ Núñez, E., Benito, C., Pazos, M. R., Barbachano, A., Fajardo, O., González, S., Tolón, R. M., Romero, J. (15 September 2004). "Cannabinoid CB2 receptors are expressed by perivascular microglial cells in the human brain: an immunohistochemical study". Synapse (New York, N.Y.). 53 (4): 208–213. doi:10.1002/syn.20050. ISSN 0887-4476.
- ↑ Mechoulam, R., ed. (1986). Cannabinoids as therapeutic agents. CRC Press. ISBN 9780849357725.
- ↑ How Marijuana Works, 2001
- ↑ Borgelt, L. M., Franson, K. L., Nussbaum, A. M., Wang, G. S. (February 2013). "The Pharmacologic and Clinical Effects of Medical Cannabis". Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 33 (2): 195–209. doi:10.1002/phar.1187. ISSN 0277-0008.
- ↑ Ärzteblatt, D. Ä. G., Redaktion Deutsches, The Therapeutic Potential of Cannabis and Cannabinoids (23.07.2012)
- ↑ Cardiovascular Effects of Cannabis | http://www.idmu.co.uk/canncardio.htm
- ↑ Is Marijuana an Effective Treatment for Glaucoma? - Medical Marijuana - ProCon.org
- ↑ Martín-Sánchez, E., Furukawa, T. A., Taylor, J., Martin, J. L. R. (November 2009). "Systematic Review and Meta-analysis of Cannabis Treatment for Chronic Pain". Pain Medicine. 10 (8): 1353–1368. doi:10.1111/j.1526-4637.2009.00703.x. ISSN 1526-2375.
- ↑ Lynch, M. E., Campbell, F. (November 2011). "Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials: Cannabinoids for pain". British Journal of Clinical Pharmacology. 72 (5): 735–744. doi:10.1111/j.1365-2125.2011.03970.x. ISSN 0306-5251.
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ Cooke, Justin (25 January 2022). "How Are Cannabinoids Metabolized? (CBD, THC, CBG, THC-O, & More)". DailyCBD.
- ↑ https://pubs.acs.org/doi/10.1021/acs.chemrestox.2c00170
- ↑ https://www.erowid.org/library/books_online/future_synthetic/future_synthetic.shtml
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ https://twitter.com/jefbev/status/1254137977933979648
- ↑ Abioye, A; Ayodele, O; Marinkovic, A; Patidar, R; Akinwekomi, A; Sanyaolu, A (31 January 2020). "Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic benefit for the management of obesity and diabetes". Journal of cannabis research. 2 (1): 6. doi:10.1186/s42238-020-0016-7. PMC 7819335
 . PMID 33526143.
. PMID 33526143.
- ↑ Brents, L. K., Reichard, E. E., Zimmerman, S. M., Moran, J. H., Fantegrossi, W. E., Prather, P. L. (2011). "Phase I hydroxylated metabolites of the K2 synthetic cannabinoid JWH-018 retain in vitro and in vivo cannabinoid 1 receptor affinity and activity". PloS One. 6 (7): e21917. doi:10.1371/journal.pone.0021917. ISSN 1932-6203.
- ↑ Coroner: Lamar Jack ingested chemical found in fake marijuana before he died » Anderson Independent Mail, 2013
- ↑ Colorado probes three deaths possibly linked to synthetic marijuana, 2013
- ↑ Synthetic cannabinoids in Europe
- ↑ Westin, A. A., Frost, J., Brede, W. R., Gundersen, P. O. M., Einvik, S., Aarset, H., Slørdal, L. (9 September 2015). "Sudden Cardiac Death Following Use of the Synthetic Cannabinoid MDMB-CHMICA". Journal of Analytical Toxicology: bkv110. doi:10.1093/jat/bkv110. ISSN 0146-4760.
- ↑ Adamowicz, P. (April 2016). "Fatal intoxication with synthetic cannabinoid MDMB-CHMICA". Forensic Science International. 261: e5–e10. doi:10.1016/j.forsciint.2016.02.024. ISSN 0379-0738.
- ↑ Trecki, J., Gerona, R. R., Schwartz, M. D. (9 July 2015). "Synthetic Cannabinoid–Related Illnesses and Deaths". New England Journal of Medicine. 373 (2): 103–107. doi:10.1056/NEJMp1505328. ISSN 0028-4793.
- ↑ Vardakou, I., Pistos, C., Spiliopoulou, C. (1 September 2010). "Spice drugs as a new trend: mode of action, identification and legislation". Toxicology Letters. 197 (3): 157–162. doi:10.1016/j.toxlet.2010.06.002. ISSN 1879-3169.
- ↑ Auwärter, V., Dresen, S., Weinmann, W., Müller, M., Pütz, M., Ferreirós, N. (May 2009). "'Spice' and other herbal blends: harmless incense or cannabinoid designer drugs?". Journal of Mass Spectrometry. 44 (5): 832–837. doi:10.1002/jms.1558. ISSN 1076-5174.
- ↑ Kronstrand, R., Roman, M., Andersson, M., Eklund, A. (1 October 2013). "Toxicological Findings of Synthetic Cannabinoids in Recreational Users". Journal of Analytical Toxicology. 37 (8): 534–541. doi:10.1093/jat/bkt068. ISSN 0146-4760.
- ↑ Mir, A., Obafemi, A., Young, A., Kane, C. (1 December 2011). "Myocardial Infarction Associated With Use of the Synthetic Cannabinoid K2". Pediatrics. 128 (6): e1622–e1627. doi:10.1542/peds.2010-3823. ISSN 0031-4005.
- ↑ McIlroy, G., Ford, L., Khan, J. M. (16 January 2016). "Acute myocardial infarction, associated with the use of a synthetic adamantyl-cannabinoid: a case report". BMC Pharmacology & Toxicology. 17: 2. doi:10.1186/s40360-016-0045-1. ISSN 2050-6511.
- ↑ 36.0 36.1 36.2 Vearrier, D., Osterhoudt, K. C. (June 2010). "A Teenager With Agitation: Higher Than She Should Have Climbed". Pediatric Emergency Care. 26 (6): 462–465. doi:10.1097/PEC.0b013e3181e4f416. ISSN 0749-5161.
- ↑ JWH-018 - Erowid Exp - “Extreme Nausea, Incoherent”
- ↑ Spice - Erowid Exp - “Playing With Fire”
- ↑ Spice and Synthetic Cannabinoids ('Drill’) - Erowid Exp - “Non-Allergic Adverse Reaction”
- ↑ published, J. B. (2010), Fake Weed, Real Drug: K2 Causing Hallucinations in Teens
- ↑ Every-Palmer, S. (October 2010). "Warning: legal synthetic cannabinoid-receptor agonists such as JWH-018 may precipitate psychosis in vulnerable individuals". Addiction (Abingdon, England). 105 (10): 1859–1860. doi:10.1111/j.1360-0443.2010.03119.x. ISSN 1360-0443.
- ↑ 42.0 42.1 Arseneault, L., Cannon, M., Witton, J., Murray, R. M. (February 2004). "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry. 184 (2): 110–117. doi:10.1192/bjp.184.2.110. ISSN 0007-1250.
- ↑ Müller, H., Sperling, W., Köhrmann, M., Huttner, H. B., Kornhuber, J., Maler, J.-M. (May 2010). "The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes". Schizophrenia Research. 118 (1–3): 309–310. doi:10.1016/j.schres.2009.12.001. ISSN 1573-2509.
- ↑ JWH-018 - Erowid Exp - “Most Insane Hour of My Life”
- ↑ AM-2201 - Erowid Exp - “The Night My Brain Caved”
- ↑ Products - Spice and Synthetic Cannabinoids (“Apocalypse”?) - Erowid Exp - “Next-Night Seizures”
- ↑ Products - Spice and Synthetic Cannabinoids ('Smiley Dog’) - Erowid Exp - “Never Again”
- ↑ Schneir, A. B., Baumbacher, T. (March 2012). "Convulsions associated with the use of a synthetic cannabinoid product". Journal of Medical Toxicology: Official Journal of the American College of Medical Toxicology. 8 (1): 62–64. doi:10.1007/s13181-011-0182-2. ISSN 1937-6995.
- ↑ Acute Kidney Injury Associated with Synthetic Cannabinoid Use — Multiple States, 2012
- ↑ Freeman, M. J., Rose, D. Z., Myers, M. A., Gooch, C. L., Bozeman, A. C., Burgin, W. S. (10 December 2013). "Ischemic stroke after use of the synthetic marijuana "spice"". Neurology. 81 (24): 2090–2093. doi:10.1212/01.wnl.0000437297.05570.a2. ISSN 1526-632X.
- ↑ Every-Palmer, S. (September 2011). "Synthetic cannabinoid JWH-018 and psychosis: An explorative study". Drug and Alcohol Dependence. 117 (2–3): 152–157. doi:10.1016/j.drugalcdep.2011.01.012. ISSN 0376-8716.
- ↑ Schneir, A. B., Cullen, J., Ly, B. T. (1 March 2011). ""Spice" Girls: Synthetic Cannabinoid Intoxication". The Journal of Emergency Medicine. 40 (3): 296–299. doi:10.1016/j.jemermed.2010.10.014. ISSN 0736-4679.
- ↑ Every-Palmer, S. (1 September 2011). "Synthetic cannabinoid JWH-018 and psychosis: an explorative study". Drug and Alcohol Dependence. 117 (2–3): 152–157. doi:10.1016/j.drugalcdep.2011.01.012. ISSN 1879-0046.
- ↑ Naphthalene - United States Environmental Protection Agency | http://www.epa.gov/ttn/atw/hlthef/naphthal.html
- ↑ Lin, C. Y., Wheelock, A. M., Morin, D., Baldwin, R. M., Lee, M. G., Taff, A., Plopper, C., Buckpitt, A., Rohde, A. (16 June 2009). "Toxicity and metabolism of methylnaphthalenes: comparison with naphthalene and 1-nitronaphthalene". Toxicology. 260 (1–3): 16–27. doi:10.1016/j.tox.2009.03.002. ISSN 1879-3185.
- ↑ Synthetic cannabinoids in herbal products (United Nations Office on Drugs and Crime) | https://www.unodc.org/documents/scientific/Synthetic_Cannabinoids.pdf
- ↑ Morris, H. (2010), HAMILTON MORRIS?: NAPTHALENE IS SO OVER